|
» Back to Table of Contents
The Challenges of Achieving
Sustained System Change
How can health care systems transform to
provide consistently safe, high-quality care
for patients as envisioned by the 2001 Institute
of Medicine's (IOM) report, Crossing the
Quality Chasm? From our research in both
VA and non-VA health care organizations,
we have identified five critical drivers of
change that distinguish organizations that
have reached sustained system change--
meaning higher levels of reliability in their
care processes and greater changes in their
systems and cultures. These five critical elements
are illustrated in the Figure below.
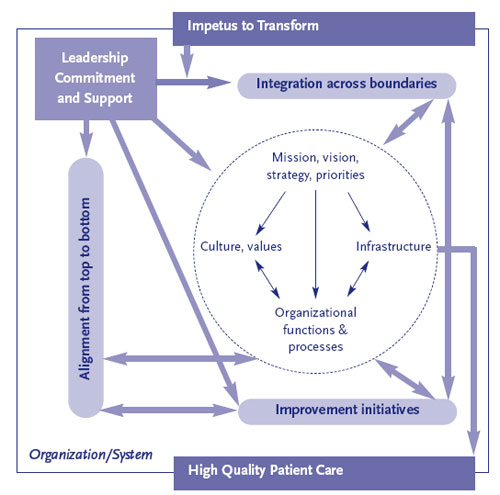
1) Impetus to transform often came from
outside the organization in response to external
pressures for change, but also came
from within the organization, often stimulated
by multiple factors. In successful transformations,
organizations sustained impetus
for change over time.
2) Leadership commitment to quality
and change -- beginning at the top of the
organization but including all levels -- proved a critical element for organizational
transformation. Senior leaders drove change
in two ways. First, they steered change
through the organization's structures and
processes to maintain urgency, set a consistent
direction, and provided resources and
accountability to support change. Second,
to create momentum for dramatic improvement
in patient care, leaders demonstrated
authentic commitment to quality, by expending
significant personal capital to motivate
staff, often leading by example through
personal involvement in improvement efforts.
3) Improvement initiatives that actively
engaged staff in meaningful problem
solving were central to change. Improvement
initiatives contributed to transformation
in at least three ways. First, initiatives
such as clinical redesign improved operations.
Second, initiatives actively engaged
staff in problem solving around meaningful,
urgent problems across disciplines and hierarchical
levels. Third, successful initiatives
built momentum for further improvement
and contributed to culture change.
4) Alignment from top to bottom to
achieve consistency of organizationwide
goals with resource allocation and
actions ensured that improvement efforts
contributed to larger system change. Accountability
was a key aspect of alignment,
ensuring that behaviors, operations, and
processes in practice supported organization-wide goals.
5) Integration to bridge traditional intraorganizational
boundaries between individual
components occurred at a later
stage of transformation. Integration is a
multi-faceted concept that applies to all organizational
levels and is both an end state
for a high-performing system and a strategy
for transformation. Integration often began
with multidisciplinary improvement teams
that encouraged communication and problem solving across work units. However, by
themselves, improvement teams ran up
against the limits of traditional organizational
boundaries. To move beyond those
limits, organizations needed integration at
the systems or organizational level in the
form of structures and processes that involved
managers with decision-making authority
and responsibilities spanning the
organization. Integrating structures and
processes also facilitated the spread of improved
clinical practices and values for improvement
across the organization.
These elements affected transformation by
driving change in complex and dynamic
health care organizations. As illustrated inside
the dotted circle in the Figure, we define
the organization, or network of
organizations comprising the system, in
terms of four basic components:
- mission,
vision, and strategies that set direction
and priorities;
- culture that reflects values
and norms;
- operational functions and
processes that embody the work that is done
in patient care; and
- infrastructure, such
as information technology and human resources,
that support delivery of patient care.
Transformation of health care systems is a
complex and difficult undertaking that is
achieved over a period of time. Each model
element offers direct practice implications
for managers seeking to change their systems
to improve patient care. However, no
single element is sufficient to achieve organizational
transformation. Managers should
recognize that all model elements are important,
and that the challenge is to maximize
the likelihood that the elements will
interact with one another in complementary
ways to maintain urgency to change and to
move the organization forward. Full transformation
may be attained only when multiple
improvements are spread across the
system and sustained over time.
Finally, successful transformation takes
time. Transformation most likely unfolds
over a decade or more. Although many of
the systems we studied demonstrated considerable
progress, they too described transformation
as a continuing journey with no
fixed endpoint. Persistence and constancy
of purpose is required for this journey.
- Institute of Medicine; Committee on Quality of
Health Care in America. (2001). Crossing the Quality
Chasm: A New Health System for the 21st Century.
Washington D. C.: National Academy Press.
- Lukas CV, et al. An Organizational Model of
Transformational Change in Health Care Systems.
Health Care Management Review, 2007; 32(4): 309-20.
|