
|
|
CommentaryTime to Use an Equity-Guided Improvement Strategy to Improve the Health of VeteransDisparities in health quality1 and safety2 are widespread in the United States. While disparities among Veterans tend to be smaller than among non-Veterans, they are not uncommon.3 For example, Black, Hispanic, and American Indian Veterans with diabetes receive needed testing, screening, and counseling at similarly high rates as white Veterans but are less likely to achieve good HbA1c or blood pressure control.4 “A rising tide lifts all boats” is often used to suggest that traditional quality improvement will eventually trickle down and equalize care for all. More commonly, groups often change in parallel, leading to the persistence of gaps. We suggest that integrating equity into quality improvement may be a more effective and efficient way to achieve change. Equity can be used to focus resources on groups in places with the worst health outcomes. It also draws attention to the centrality of not delivering more services but delivering services in a way that optimizes health for patients. Recent research demonstrates that quality improvement strategies can be applied to reduce disparities within VA facilities serving very different populations.5 It is time to use quality improvement more broadly to reduce disparities and achieve health equity for Veterans. An Equity-Guided Improvement Strategy is an approach for identifying specific groups of Veterans receiving care in specific VA facilities who are not achieving equitable health outcomes. It can be used to assess whether underperformance in a facility on a particular metric is evenly distributed across a patient population (Homogeneous Population) or underperformance is largely attributable to care received by specific groups (Heterogeneous Population). 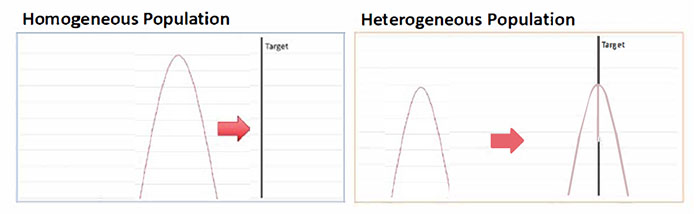
This distinction may have important operational implications. If underperformance is evenly distributed across a homogeneous population (Figure, left), traditional quality improvement techniques, which typically take a one-size-fits-all approach, can be applied to redesign care processes and raise average performance to the target level. However, in a heterogeneous population (Figure, right), some groups may already be at target, so altering care processes for them may be unnecessary and disruptive. Instead, care processes that work for groups at target may need to be adapted and translated to work with groups that are below target. For example, dietary counseling that works well for middle-class Veterans with adequate transportation may need to be adapted for Veterans with lower incomes with less access to transportation and take into account the local food environment where Veterans live. In addition, limited quality improvement resources can be focused on just the groups that are below target. Rather than modifying care processes for all patients, effort can be concentrated on enhancing care for the subset farthest from the target. An Equity-Guided Improvement Strategy is appropriate for improving care in many VA facilities. For example, most serve large numbers of Veterans of Color. In 96 percent of VA hospitals, minority Veterans make up 10 percent or more of patients served; in 18 percent of VA hospitals, the majority of Veterans served are People of Color. In most VA facilities, disparities are not uncommon. We estimate that in over a quarter of all VA hospitals, more than half of the underperformance in control of diabetes or hypertension can be attributed to care received by either Black or Hispanic Veterans. Quality improvement efforts that focus on delivering culturally sensitive counseling to these Veterans in these VA facilities may yield better results than traditional quality improvement. An Equity-Guided Improvement Strategy is also appropriate in the current pandemic. As in the general population, Veterans of Color are experiencing a disproportionate share of COVID-19 cases likely due in part of their service as essential workers and in other jobs that make social distancing more difficult, and to their residence in high density neighborhoods and multigenerational households.6 In addition, Veterans of Color tested for COVID-19 at VA are more likely to test positive, suggesting that they are facing greater barriers to testing. We identify specific counties served by VA facilities in which Veterans of Color have particularly high positive test rates (COVID Equity Reports, updated through 6/30/2021) (available only within VA). Tailored messaging to Veterans of Color in these neighborhoods may help them overcome barriers to testing and encourage them to come to VA for COVID-19 care and eventual vaccination. Free of profit motive, able to address many of the social determinants of health that adversely affect Veterans, and rich in data and dedicated providers, VA is ideally situated to use an Equity-Guided Improvement Strategy to ensure equitable outcomes for all who served. Such an approach can help us ensure that all Veterans receive the information, care, and support they need in the current crisis and for the rest of their lives.
For more information on using an Equity-Guided Improvement Strategy, see the Office of Health Equity SharePoint at Equity Tools [VA Intranet only – link will not work outside VA]
. Start with the
3-minute video, "Engaging Healthcare Teams to Eliminate Health Inequities", developed by the HSR&D Center for Health Equity Research and Promotion. Then, explore the dashboards.
References
|
|
Next ❯