
|
|
Research HighlightMeeting the Needs of Transgender and Gender Diverse Veterans: Research Can Help Move VHA ForwardKey Points
The term transgender refers broadly to people whose gender identity differs from the sex assigned to them at birth. The Veterans Health Administration (VHA) LGBTQ+ Health Program has adopted the phrase “transgender and gender diverse” (TGD) to acknowledge and encompass the diversity of identities and expression among the Veterans that VA serves. Research about TGD individuals has revealed alarming disparities across several medical conditions (e.g., cardiovascular disease), behavioral risks (e.g., attempted suicide), and social environmental factors (e.g., housing instability) that jeopardize health and well-being. Understanding the unique needs of TGD Veterans who utilize VHA care has been challenging, primarily due to the inability to identify representative samples in healthcare data. Self-identified gender identity – the gold standard assessment – has not historically been collected in VHA’s administrative or electronic health records, forcing reliance on proxy methods, such as International Classification of Disease (ICD) diagnostic codes used for treating gender dysphoria, in order to conduct research. Through this method, VHA’s health equity research portfolio corroborated findings from studies of non-Veteran TGD individuals, and propelled novel studies that filled crucial gaps in knowledge. For example, studies of VHA TGD Veterans have found high rates of suicidal ideation and suicide attempts, which have commonly been documented among TGD people. However, the linkage of VHA’s Corporate Data Warehouse data with National Death Index data, curated through VHA’s Mortality Data Repository, enabled the first comparative study of mortality among a sample of TGD people in the United States.1 The findings showed that despite death by suicide being high among all Veterans, TGD Veterans in VHA had over twice the risk of suicide death than cisgender (non-TGD) Veterans. Moreover, on average, TGD Veterans are dying by suicide at younger ages than their cisgender peers (52 years versus 64 years, respectively), resulting in greater burdens of years of potential life lost to suicide. Additionally, TGD Veterans were over three times as likely to die from homicide than cisgender Veterans; although it should be noted that the estimates were unstable because of the rarity of homicide documented on death certificates. These results confirmed, for the first time, that one of the main public health metrics to gauge community health (i.e., cause-specific mortality) signaled dire disparities for this marginalized population of Veterans. Discovering drivers of these disparities led to additional VHA research focused on social determinants of health. TGD people appear to experience relentless stigma, including violence, family estrangement, being fired from jobs, and legislative discrimination about what bathrooms they can use or sports they can play. These social adversities endanger health and promote financial strain and housing instability. For instance, housing instability is nearly three times more prevalent among TGD VHA Veterans than non-TGD VHA Veterans. Also, approximately one-third of TGD VHA Veterans had an indicator of financial instability in their medical records and nearly 15 percent screened positive for military sexual trauma.2 These studies underscore the importance for VA health services researchers to understand the social and structural factors that can both directly and indirectly impact the individual-level health of TGD Veterans. As research has illuminated social and structural threats to TGD Veterans’ health, over the last decade there have been structural changes to the VHA health system to improve the lives of TGD Veterans. Principal among these changes was VA’s national directive about healthcare for TGD Veterans in 2011. Shortly thereafter, the establishment of the LGBTQ+ Health Program in VA Central Office created the foundation for several clinical education, training, and resource initiatives. Virtual training through Specialty Care Access Network for Enhancing Community Health Outcomes (SCAN-ECHO), resulted in nearly 900 providers receiving intensive training in TGD healthcare, including gender-affirming hormone therapy. The VHA LGBTQ+ Health Program created a formal e-consultation service on TGD healthcare in 2015, allowing VA providers to receive advice from experts. In 2016, LGBTQ+ Veteran Care Coordinators were appointed at every VA medical center to help ensure care delivery is inclusive and affirming. In 2020, a project to provide nationwide access to gender-affirming vocal coaching through telehealth was launched, which assures that rural TGD Veterans have access to these specialty services. In 2021, a rule change process was initiated to remove a ban on transition-related surgical procedures, which will enable eligible TGD Veterans to receive safe and equitable care. Despite progress, substantial research challenges remain to better meet the needs of TGD Veterans. We highlight two of those challenges here. First, enabling VHA to capture self-identified gender identity from patients would provide health services researchers an alternative to relying on ICD codes. ICD codes are problematic for several reasons, including characterizing a person’s gender identity as a medical condition and missing TGD Veterans without ICD codes related to gender dysphoria, resulting in underreporting TGD Veterans in VHA research. Second, engaging TGD Veterans in the research process and in primary data collection is crucial for patient-informed, and ultimately patient-centered, research. Through qualitative interviews with 30 TGD Veterans, we are learning more about the requests – and requirements – that researchers need to be prepared to meet in forging these partnerships. Preliminary findings demonstrate that researchers should be prepared to involve TGD Veterans in all phases of the study, clearly communicate the research team’s intentions, ensure the confidentiality of TGD identity and that participation will not impact VA care, mitigate potential harms of research, and make research participation convenient (Figure 1). 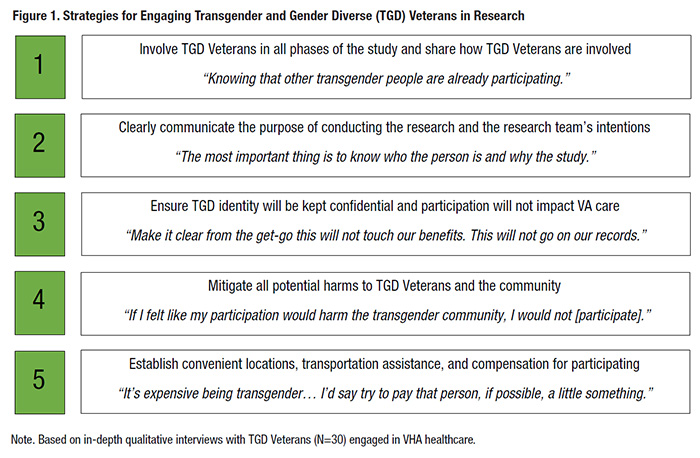
The TGD population in VHA is rapidly growing and has nearly doubled since 2014 when there were about 5,000 TGD Veterans in the VHA population.3 VHA researchers, along with operational partners, are trying to better understand how to improve the lives of TGD Veterans we serve. The breadth of needed research is vast – ranging from reproductive health, to effective suicide prevention, to the long-term effects of gender-affirming hormones. Improving the approaches to addressing TGD Veteran health inequities by increasing data collection on gender identity and working with TGD Veteran stakeholders are critical. Using commitment to health equity as a guide, VHA can become a national leader for high-impact research that reduces disparities, improves healthcare, and promotes well-being for TGD Veterans. References
|
|