
|
|
Response to CommentaryInvestments in Multidisciplinary Research Are Foundational to Reduce Preventable Harm to PatientsHealth Services Research (HSR) conceptual models examine the complexity and “basic science” of patient safety. HSR methods can help quantify patient safety problems, enhance their understanding, and develop and test solutions. However, preventable harm persists and even worsened during the pandemic. One reason is inadequate attention and investment in patient safety over the past two decades. Significant investments are still needed to measure the burden of different patient safety events across settings and to address emerging safety threats. Solutions need to be developed, evaluated, and implemented through rigorous research to ensure widespread, effective adoption. Multidisciplinary strategies are required both to mitigate safety threats before they lead to patient harm, and to close the implementation gap. Outside of AHRQ and VA funding, patient safety research in the United States is underfunded. Efforts to translate HSR to patient care, policy, and clinical practice is essential for patient safety improvements. These efforts require health services researchers to go beyond publishing a paper; they must work closely with healthcare organizational leaders, clinicians, policymakers, and patients to ensure their findings are acted upon, and to help propose and test solutions. Funding for Centers of Excellence that leverage multidisciplinary teams using different technical, social, psychological, organizational, and clinical perspectives is needed to address complex sociotechnical safety problems and deepen the impact of HSR (Figure 1). The commentary by Mills, et al. highlights how the National Center for Patient Safety (NCPS) offers an excellent model to do so by funding dedicated patient safety centers of inquiry (PSCIs) nationally. PSCIs focus on research and implementation activities that promote organization-wide learning. The PSCI model adds significant value to creating a learning health system for safety that invests in patient safety data gathering, analysis, learning, and actionable improvements. Centers focus on scholarly and implementation activities that strategies to the bedside. Our research team has been funded by NCPS as a PSCI since 2007. Back then, funding for the underemphasized topic of missed and delayed diagnosis was hard to obtain. Evidence of both problems and solutions was anecdotal and diagnostic safety science was not as robust. These limitations made it harder to obtain research funding, and there were fewer opportunities for early career researchers. Thus, the 2006 call for patient safety centers of inquiry proposals was a landmark event for our team. We imagined a PSCI that leveraged informatics, social science, cognitive science, and human factors engineering to improve the safety of EHR-based communication, specifically test results and referrals. The Houston VA Health Services Research & Development Center for Innovations in Quality, Effectiveness and Safety has housed and supported the PSCI activities. Our PSCI’s work confirmed that diagnostic errors are common and harmful and should be prioritized in all patient safety improvement initiatives. In subsequent PSCI iterations, we continued to focus on diagnostic errors within one specific context: failure to follow up abnormal test results communicated through VA’s EHR, also referred to as “missed test results.” Our work has been considered significant by both VA and non-VA audiences, with a high potential for clinical impact, as evidenced by the rapid translation of our findings into deliverables to improve safety. For instance, our team developed several types of innovations useful for practice, including e-triggers1 (electronic algorithms that detect potential safety events) and SAFER Guides – guides or EHR safety assessment, which have been adopted by the Centers for Medicare & Medicaid Services as a requirement for all hospitals. Our team also developed an EHR-based decision support tool for reducing missed test results and recommended several practical strategies to improve the safety of EHR-based communication. During our work, we intervened in hundreds of situations to prevent patient harm from missed test results. In one instance, we discovered and corrected an EHR software problem that had caused multiple breakdowns in communication of test results. We also developed and disseminated nationally a toolkit to improve the communication of test results and two toolkits for enhancing the management of EHR-based inbox notifications (View Alerts), one of which is now used for clinician training by many VA sites. Our work has also influenced VA policy on test results communication to clinicians and patients. The latest revision of Directive 1088 on Communicating Test Results to Providers and Patients sets standards for the timeliness of communicating test results depending on whether they are actionable. Based on this policy and our team’s work, VA developed new performance indicators of timely communication of test results along with quality measurement guidance for data collection through the External Peer Review Program.2 We are now developing strategies to export multiple e-triggers to help others implement them, and to leverage the knowledge gained from the e-triggers to improve diagnostic safety in VA. Progress towards reducing diagnostic errors will hinge on our ability to facilitate such measurement for learning and improvement at local VA sites. Because many processes in VA are centralized and our EHR data repository is national, NCPS support provides us with the potential to have our work implemented and translated across the VA system, especially as VA transitions to Oracle-Cerner EHR. While we still have miles to go in improving diagnostic safety and more investments are needed, the PSCI mechanism has positioned us well to make a broad impact on national policies and procedures in VA. PSCIs can accelerate the impact of multidisciplinary science in enhancing the understanding of the complexity of patient safety as well as developing and testing solutions. This is a promising pathway to prevent patient harm and transition from a “Bronze Age of rudimentary tool development to a Golden Era of vast improvement in patient safety.”3 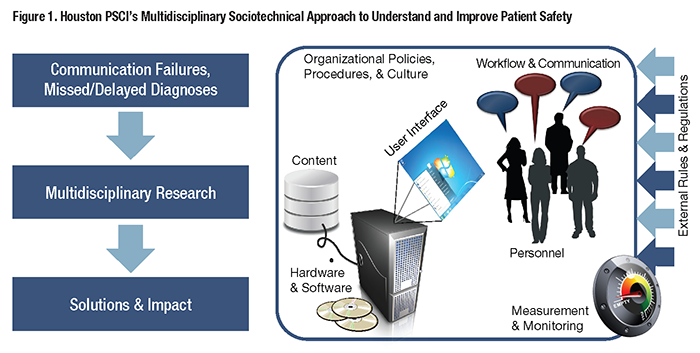
References
|
|