
|
|
Research HighlightCaregiver Survey Reveals Opportunities to Leverage Family Caregivers as a Clinical ResourceKey Points
In the United States, family caregivers form the backbone of the long-term care system, with an estimated 5 million individuals providing often unpaid care for aging and disabled Veterans.1 VA provides the only national, comprehensive support program for family caregivers in the country. In 2010, Congress authorized the Program of Comprehensive Assistance for Family Caregivers (PCAFC) for family caregivers of Veterans who served post-9/11 and were injured during their time of service. This program provides a monthly stipend, education and training, mental health care, respite care, and other services.1 Evidence suggests that PCAFC caregivers help Veterans access high-value care; navigate the health care system; advocate for Veteran needs; and provide a bridge between home and clinical care.2 The 2018 MISSION Act expanded eligibility for PCAFC to include caregivers of Veterans who served in pre-9/11 eras. However, little is known about this potentially eligible group of family caregivers. Methods and ResultsAs part of an ongoing evaluation of the VA Caregiver Support Program,i 1,507 caregivers of pre-9/11 era VA users participated in a survey about their demographics, health status, caregiving tasks, caregiver burden, and experiences with VA. Figure 1 describes the characteristics of these caregivers. Two-thirds of respondents reported that Veteran care recipients experienced total impairment in activities of daily living—meaning that they could not independently perform 8 out of 13 activities of daily living (e.g. bathing, dressing, grocery shopping). The top five Veteran health problems requiring a caregiver were, in rank order: depression, other physical illness or injury, anxiety, posttraumatic stress disorder, and Alzheimer’s disease or dementia. Respondents reported providing high intensity care on most days of the week (mean 6.7 days) and during many hours of the day (mean 9.6 hours/day). Respondents reported long duration of caregiving—over six years on average. Prevalence of distress and burden among caregivers was also high. The average Center for Epidemiologic Studies Depression Scale (CES-D) score was 11.5; a score ≥8 indicates probable depression. The mean Zarit burden score was 21.8; a score ≥16 suggests clinically significant subjective burden. A large proportion of respondents also reported high levels of financial distress and feelings of social isolation (Figure 1). Caregivers also evaluated their experiences with the VA healthcare system. On average, survey participants rated the quality of their Veterans’ health care at VA in the last three months as 8.1 out of 10, where 0 indicates the worst and 10 the best possible care; 35 percent rated the health care their Veteran received at VA as the “best possible” (e.g. a score of “10”). When asked about health care received in the last six months, 51 percent of caregiver respondents believed that the Veterans’ health care teams understood what mattered most in terms of the care provided to their Veteran, while 43 percent stated that the health care team never talked to them about community or home-based services to support the Veteran. Implications for the MISSION ActSurvey respondents were primarily wives providing care to their Vietnam-era Veteran husbands who had substantial functional and cognitive impairment and heavy mental health burden. The vast majority of caregivers experienced significant mental health distress, financial strain, and burden related to caregiving. Rates of depressive symptoms are particularly concerning; 57 percent of our survey respondents versus 19 percent of pre-9/11 caregivers surveyed by RAND reported symptoms of probable depression.1 These findings suggest family caregivers who are potentially eligible for PCAFC through the MISSION Act are an especially distressed population in need of emotional support, respite care services, and training in disease education and clinical skills to help manage the emotional and physical aspects of caregiving. Preliminary evidence suggests that PCAFC may reduce negative effects of caregiving on the caregiver.3 The MISSION Act also mandates that PCAFC offer new services, e.g. financial planning; thus, the expansion of PCAFC and additional features are highly relevant to caregivers of pre-9/11 Veterans. Despite respondents’ favorable rating of VA quality of care, a large proportion of caregivers reported that the Veterans’ health care teams do not adequately engage them or provide referrals for community-based supports and services. As members of the health care team that bridge clinical and home care, caregivers might improve quality of care for Veterans; and our results suggest that the VA health care system may be missing the opportunity to leverage family caregivers as a clinical resource. The Elizabeth Dole Foundation’s Campaign for Inclusive Care has partnered with VA and identified provider education as one potential strategy to integrate caregivers into the care team. As part of the impetus around the MISSION Act, VA could expand efforts to educate providers about family caregivers as a clinical resource and inform them of the high distress caregivers experience while caring for Veterans. 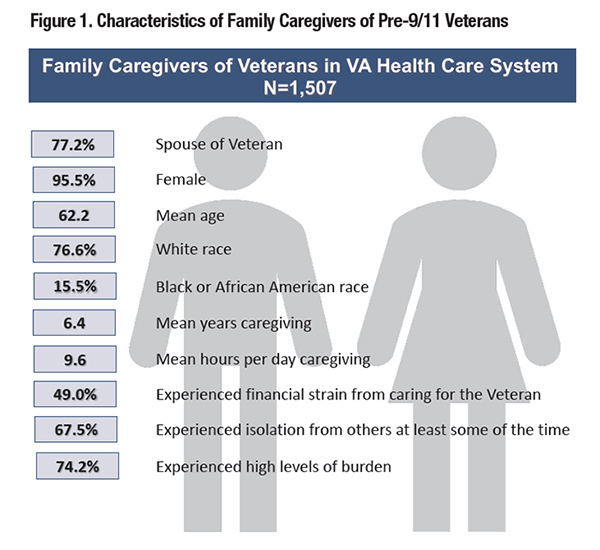
References
|
|