
|
|
Organizational ProfileMultidisciplinary Center Builds Evidence to Keep Veterans at Home While Engaging and Supporting CaregiversThe Elizabeth Dole Center of Excellence for Veteran and Caregiver Research was created in October 2018 as part of the VA Choose Home Initiative. The goal of Choose Home is to allow Veterans to remain in their homes rather than institutional care. The Center expands VA capacity to deliver integrated, Veteran and caregiver-partnered, data-driven approaches to care. Named in honor of Senator Elizabeth Dole in recognition of her significant efforts to highlight the needs of caregivers, the Center is funded through the VA Health Services Research and Development service for five years. Senator Dole’s work to shine a spotlight on the needs of caregivers culminated in the “Hidden Heroes” RAND report demonstrating the extent of caregiving in this country. The Dole Center of Excellence Team is a virtual one, comprised of a multidisciplinary group of researchers and clinicians from across the country, many of whom are Veterans, caregivers, and survivors themselves. Our four primary sites include Miami, Palo Alto, Salt Lake City, and San Antonio, in collaboration with the Geriatrics and Extended Care Data Analytics Center (GECDAC). The four sites include Geriatric Research, Education, and Clinical Centers; our investigators are also members of two VA HSR&D Centers of Innovation. The Dole Center offers a fellowship program that supports fellows at each of the four sites; the fellows program is open to all health professions, and is overseen by Dr. Sandra Sanchez-Reilly. Center activities are organized around three cores: innovation, outcomes and implementation, and data and policy. The figure below shows the organization of the Center team. The innovation core, overseen by Dr. Stuti Dang in Miami, is comprised of four pilot projects. The San Antonio pilot led by Dr. Carolyn Pickering will evaluate the impact of a hands-on caregiver skills training program. In Miami, a refined primary care model tailored to the needs of high-need, high-risk Veterans who do not need home-based primary care is being evaluated by Dr. Stuti Dang. Palo Alto investigators Dr. Ranak Trivedi and colleagues will examine Veteran and caregiver use of community resources through assessing barriers to use, particularly for specific Veteran and caregiver groups, and evaluating the impact of integrating resource linkages into caregiver-Veteran support programs. Finally, Dr. Rand Rupper in Salt Lake City is leading an evaluation of integrating dynamic assessment of functional status into decision support at the point of care. The outcomes and implementation core, overseen by Dr. Erin Finley in San Antonio, has two sets of activities. The first is to partner with Veterans, caregivers, and stakeholders to develop a group of harmonized outcome measures that are most meaningful to these groups. The team has conducted an environmental scan of currently used assessment tools, convening focus groups and interviews to evaluate potential measures. Our preliminary findings suggest that caregivers would like to see measures related to resource helpfulness and ease of system navigation, particularly with regard to their ability to connect with community resources. The second activity of this core is conducting an ongoing evaluation of the pilot projects based on the “replicating effective programs” model to obtain information that would support widespread implementation of successful practices. Finally, the data and policy core, overseen by Dr. Mary Jo Pugh in Salt Lake City, is conducting a data analytics project to determine what types of non-institutional care are most effective in preventing institutionalization for different Veteran populations. The analytic team is coordinating with the GECDAC and with Dr. Jim Rudolph, Director of HSR&D’s Long Term Support Services Center of Innovation, to ensure that our findings are aligned with other work in this area. Our study team will then integrate findings across these research activities to develop a set of recommendations and tools for operational partners and policy makers. At the end of five years, we hope to have produced knowledge that helps keep Veterans at home, and that engages and supports caregivers. Our research kickoff meeting held in January 2019 included VA researchers Dr. Nina Sperber from Durham, Dr. Alison Hamilton from Los Angeles, and Dr. Jim Rudolph from Providence, Dr. Tom Edes from Geriatrics and Extended Care, Dr. Ben Kligler from the Office of Patient Centered Care and Cultural Transformation, and Drs. Orna Intrator and Bruce Kinosian from the Geriatrics and Extended Care Data Analytics Center, allowing us to refine our research plans to best align with other work being conducted across VA. While operating a virtual center across multiple sites has its administrative challenges, working with this outstanding research team has been a wonderful experience for all of us. The opportunity to partner with Veterans and caregivers on our research program adds to the meaning of our work. Our team has been fortunate to work closely with the Veterans Experience Office, under the tremendous leadership of Dr. Lynda Davis, and with Dr. Amy Kilbourne, Director of the Quality Enhancement Research Initiative in HSR&D. We are appreciative of the support from both of these leaders. We also thank Dr. George Fitzelle, who has been an incredibly helpful partner in his Scientific Portfolio Manager role. 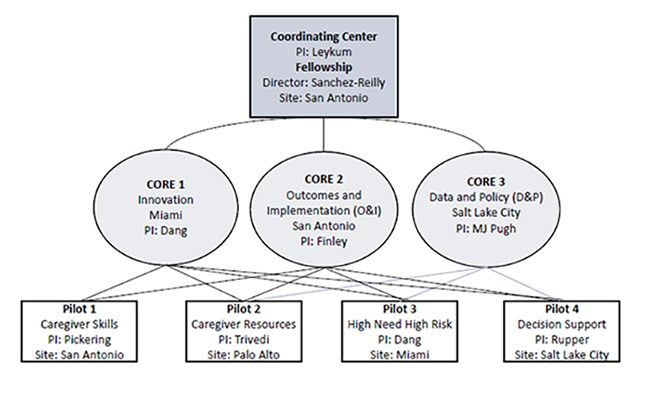
|
|