
|
|
Research HighlightEngaging Women Veterans in Evidence-based Care: VA EMPOWER QUERI 2.0Key Points Women Veterans are the fastest-growing segment of users in the Veterans Health Administration (VA), with their numbers projected to increase by 73 percent, from 9 percent to 16 percent of all Veterans, between 2015 and 2043. In anticipation of this increase and in response to women Veterans’ unique and complex healthcare needs, VA has invested heavily in delivering care for women Veterans that is effective, comprehensive, and gender tailored. Ample research suggests that a sizeable proportion of women Veterans have yet to feel that VA is their “medical home.” Women Veteran non-VA users perceive VA care quality to be inferior, and the rate of attrition among women Veterans who seek VA care is alarming. To help address these critical gaps, we focused our efforts on improving women Veterans’ engagement and retention in VA care. We conceptualize engagement as “patients, families, their representatives, and health professionals working in active partnership at various levels across the healthcare system – direct care, organizational design and governance, and policy making – to improve health and health care.”1 In VA, promoting patient engagement may be especially useful in improving quality of care among high-risk or under-represented populations, such as women Veterans, especially those who might be isolated from care due to geography and other factors, such as disability. EMPOWER QUERI 1.0Since its inception in 2015, the Enhancing Mental and Physical health of Women through Engagement and Retention (EMPOWER) QUERI 1.0 team has focused on implementing gender-tailored, preference-based care models for women Veteran patients with high-priority health conditions: 1) prediabetes, 2) cardiovascular risk, and 3) anxiety and/or depression.2 In EMPOWER 1.0 studies of evidence-based practices addressing these conditions, women expressed preferences for gender-specific care and for virtual care.3 We also found that women Veterans saw benefits from participation in virtual care; for example, women who enrolled in the virtual gender-tailored Diabetes Prevention Program (DPP) had higher rates of participation (66 percent vs. 27 percent completed ≥9 sessions/modules) compared to those enrolled in in-person DPP. Overall, our findings across three interventions convinced our team and our operations partners that we need to increase access to virtual care and focus more intensively on prevention, especially given that women Veterans might be using VA across their lifespan. EMPOWER QUERI 2.0In EMPOWER 2.0, we have extended our overarching commitment to improving women Veterans’ engagement and retention in care by expanding access to virtual, evidence-based, preventive services for women Veterans across four VISNs. We continue to focus on women’s high-priority health conditions, specifically prediabetes, cardiovascular risk, and perinatal depression. In collaboration with our seven VA operations partners, we are supporting implementation of three evidence-based practices (EBPs): 1) gender-tailored DPP (to prevent diabetes), 2) Telephone Lifestyle Coaching (TLC, to prevent cardiovascular disease), and 3) Reach Out, Stay Strong Essentials (ROSE, to prevent perinatal depression). DPP, an evidence-based lifestyle intervention emphasizing moderate weight loss, diet, and >150 minutes of physical activity per week, has been shown in randomized trials to prevent and/or delay progression to diabetes. Virtual DPP, which includes small, closed virtual groups and human coaches, is recommended by the CDC, meets U.S. Preventive Services Taskforce recommendations for care of persons at risk for diabetes, and adds to the menu of available VA weight management services. Developed by one of our operations partners, the National Center for Disease Prevention and Health Promotion (NCP), TLC is a theory- guided program involving virtual (telephone-based), individual-level, personalized health coaching focused on disease prevention and wellness. Pilot studies of TLC found strong engagement among women Veterans as well as statistically significant weight loss and high satisfaction among Veterans and VA staff. ROSE is an evidence-based intervention (studied in five randomized controlled trials) for preventing post-partum depression (PPD) among racially and ethnically diverse low-income women at high risk for PPD. In a systematic review of preventive interventions for perinatal depression in pregnant and post-partum women, the U.S. Preventive Services Taskforce found that ROSE reduced the relative risk of perinatal depression by 53 percent. To support site implementation of these EBPs, we are using two well-established implementation strategies: Replicating Effective Practices (REP) and Evidence-Based Quality Improvement (EBQI). Within VISNs, sites are randomized to one of these strategies and we are evaluating several outcomes related to engagement in care, as well as cost and return on investment. To date we have randomized 20 sites, interviewed 106 key stakeholders, trained 42 VA staff in EBQI, trained 39 VA staff in ROSE, and launched the EBPs in eight sites, with the remaining sites preparing for implementation. We have developed a Power BI dashboard for each site to understand site-specific population characteristics, explore performance measures, and monitor implementation. In addition, we support time-sensitive requests from our operations partners for rapid response projects; in fiscal year 2022, we conducted a qualitative evaluation of VA women’s mental health champions’ experiences and impacts of their roles for the Office of Mental Health and Suicide Prevention, and an evaluation of VA-provided childcare services for the Office of Women’s Health. The EMPOWER TeamOur approach to improving women Veterans’ access to and engagement in care would not be possible without a diverse team of clinicians, implementation scientists, social scientists, and experienced VA staff, including Veterans. Four PIs and three Co-PIs lead the initiative: Drs. Bevanne Bean-Mayberry, Melissa M. Farmer, Erin Finley, Alison Hamilton, Sally Haskell, Ariel Lang, and Tannaz Moin. Our national operations partners, Technical Expert Panel, VISNs, and the VA HSR&D Women’s Health Research Network guide our efforts and ensure consistent alignment with VA policy priorities. 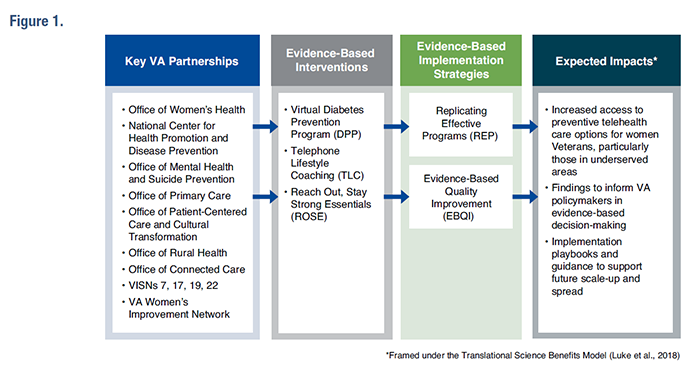
References
|
|