
|
|
Research HighlightVA's Maternity Care Coordinator Telephone Care Program: A Model for Coordinating VA Specialty Care in the CommunityKey Points VA maternity care is almost entirely provided by non-VA providers and, as such, presents challenges to coordinating the care of pregnant Veterans across healthcare systems.
The MISSION Act of 2018 and the preceding Access, Choice and Accountability Act of 2014 require that the Veterans Health Administration (VA), under pre-specified conditions, pay for Veterans to receive care from non-VA providers. While enhancing the range of care options available to Veterans, these new arrangements also present a multitude of challenges due to the complexity of coordinating Veterans’ care needs across healthcare systems. 1 For women Veterans, however, the dual use of VA and non-VA healthcare is not new, nor is the need for coordinating their care across healthcare systems. As a numerical minority, gender-specific specialty services for women are often not available within VA. 2 In such cases, VA pays for women Veterans to receive this care from non-VA providers. A prime example is VA maternity care, a benefit that has been available since 1996, but is provided almost entirely by non-VA providers. 3 Although pregnant Veterans receive their maternity care from non-VA providers, they continue to use VA providers for treatment of their mental and non-obstetric physical health conditions. In our care coordination needs assessment, we found that among 244 pregnant Veterans, 41 percent had pre-pregnancy chronic physical conditions and 34 percent experienced mental health problem(s).3 Therefore, concurrent use of VA and non-VA services is common among pregnant Veterans, and care coordination is critical for ensuring that pregnant Veterans get the time-sensitive care they need. To address these coordination needs, VA established a national maternity care coordination policy in 2012, which requires that each pregnant Veteran using VA maternity benefits be assigned a maternity care coordinator (MCC). VA developed the MCC Telephone Care Program (MCC-TCP) to provide support for MCCs in delivering effective care management for pregnant and post-partum Veterans using VA maternity care benefits.3 MCC-TCP consists of eight scheduled telephone calls with Veterans, covering 12 topics, as summarized in Figure 1 below.Some topics are covered with every Veteran, and others are covered only if appropriate for the Veteran’s needs (e.g., smoking cessation). Some topics are covered once (at the pregnancy stage when they are appropriate), and others are repeated across calls. During all telephone calls, MCCs address questions related to VA maternity care benefits and coordination of care for chronic illnesses. Between scheduled telephone calls, the MCC is available to the Veteran as needed and makes additional (unscheduled) telephone calls to follow-up on problems identified during the scheduled calls. MCCs utilize checklists to guide each call, templates to document the calls, and electronic logs to track the calls and care coordination tasks. To implement and spread MCC-TCP, we constructed a manual with checklists and sample scripts for each call, conducted live interactive training sessions to educate the MCCs on program components, and recorded a 10-session internet-based education series (available “on demand”) covering foundational maternity care coordination knowledge (e.g., overview of testing during pregnancy). To assist MCCs in determining local variations in their VA’s resources and processes related to maternity care, we provided MCCs with a “Resources and Processes Workbook.” We formatively evaluated MCC-TCP by tracking Veteran participation, as well as MCC perceptions captured through surveys, implementation meeting field notes, and MCC time logs. We used the results of the formative evaluation to make improvements to the program. For example, based on feedback from the evaluations, we developed both the Resources and Processes Workbook and the foundational knowledge educational series; we also made extensive modifications to the call checklists, logs, and sample scripts. The formative evaluation of barriers to implementation also revealed that the MCCs felt they lacked adequate time to coordinate pregnant Veterans’ care optimally. Time logs showed that MCCs spent 150 minutes on average per pregnant Veteran. MCCs spent over one-third (38 percent) of this time making the phone calls (including leaving messages), while MCCs spent 23 percent of this time reviewing charts in preparation for calls, 27 percent documenting calls, and 12 percent performing other care coordination activities. Many MCCs delivered MCC-TCP while performing collateral clinical duties and reported they had inadequate time for their MCC role. MCCs also reported frustration with the amount of time they spent attempting to reach Veterans by phone, sometimes unsuccessfully. During our implementation evaluation period, MCCs completed 60 percent of attempted scheduled calls. For the remaining scheduled calls, MCCs either could not reach the Veteran or the Veteran was not available. MCCs generally make multiple attempts to reach Veterans for each scheduled call. Despite these challenges, MCCs reported that they perceived MCC-TCP as being highly valuable for coordinating pregnant Veterans’ care. MCC-TCP provides a model for coordinating care for all Veterans, male and female, who are simultaneously receiving VA and non-VA care. Development and implementation of MCC-TCP offers important insights relevant to future endeavors. First, care coordination can be time-intensive, and caution should be taken to provide coordinators with adequate time to perform this work. The efficiency, and potentially the effectiveness, of these coordination tasks would likely be greatly enhanced with investments in developing and testing asynchronous communication technologies, such as mobile health applications, rather than continuing to rely exclusively on telephone calls. Finally, it is hard to overstate the extent of variations across VA sites in the resources and processes relevant to providing and coordinating care. The extent to which care coordination programs can be flexible to accommodate these variations is key to their implementation and sustainability. 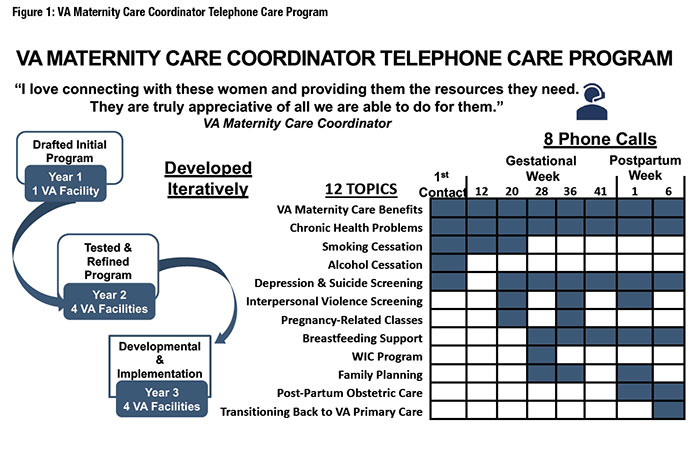
References
|
|
❮ Previous