|
» Back to Table of Contents
Key Points
- Veterans with existing mental health conditions as well as Veterans from vulnerable subgroups may be at heightened risk for adverse mental health outcomes during the COVID-19 pandemic.
- With release of a Rapid Response RFA in Spring 2020, HSR&D sought to accelerate research efforts that would inform
short-term decision-making and long-term planning for a research agenda focused on the mental health impacts of the pandemic.
- This article provides an overview of eight HSR&D-funded Rapid Response studies that address mental health and care delivery in the wake of the pandemic.
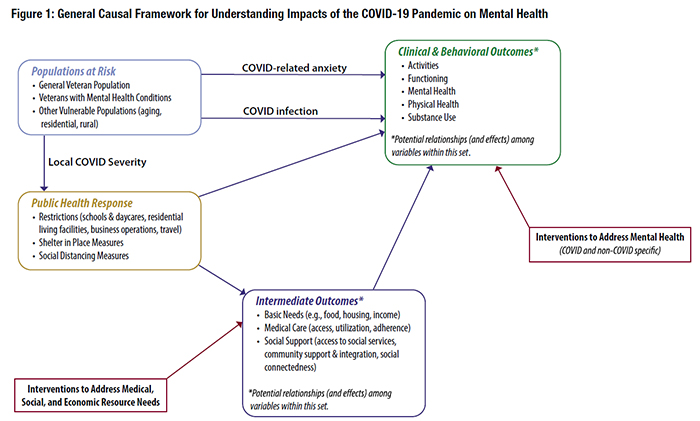
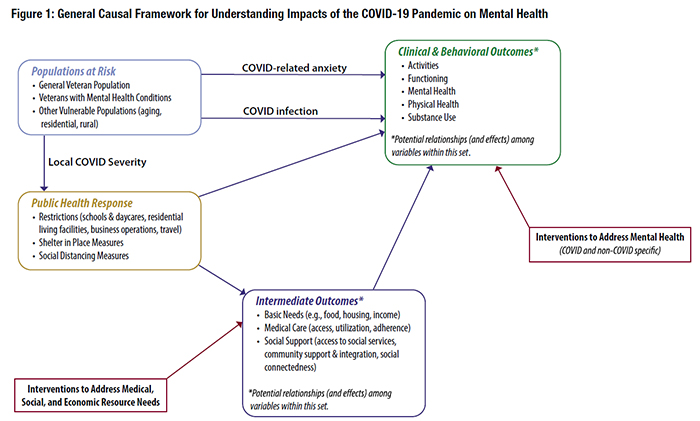
Past experience and emerging evidence portend significant mental health impacts from the COVID-19 pandemic, including elevated levels of anxiety, depression, psychological distress, substance use, and suicidal ideation.1 These mental health impacts (new cases and/or worsening of existing conditions) are hypothesized to result (directly or indirectly) from the public health measures needed to mitigate the spread of the virus (e.g., physical distancing, lockdowns, school closures) (Figure 1). Veterans with existing mental health conditions, as well as those from vulnerable subgroups (e.g., aging, homeless, residential rehab, rural), may be particularly at risk for adverse mental health outcomes during the COVID-19 pandemic.
Addressing the mental health impacts of the COVID-19 pandemic in a robust, effective manner requires strategies that can support a research agenda that includes analyses to inform decision-making on a relatively short timeline; studies that guide long-term planning; and projects to understand the unique conditions of the pandemic (and what works under these conditions).2 HSR&D released a Rapid Response RFA (Spring 2020) to jumpstart research efforts in these domains, including data analysis projects; planning projects (“preparatory to research”); and short-term pilots. This funding mechanism allowed for timely, targeted, and coordinated work to build partnerships, develop capacity, and conduct foundational research and operations work necessary to address critical questions surrounding the COVID-19 pandemic. HSR&D received and reviewed over 200 proposals under this RFA, and within three months of submission, funded 21 new studies and 5 supplements to existing awards, 8 of which addressed mental and behavioral health and care delivery issues.
As outlined below, the COVID-19 mental health research projects funded by HSR&D address a broad range of Veteran-centric topics, from social distancing to access to care to an after-action review of the COVID-19 response.
- Bryann DeBeer (Aurora, Colorado): Impact of COVID-19 and Social Distancing on Mental Health and Suicide Risk in Veterans. This cross-sectional study uses social network analyses to examine pandemic-related changes to Veterans’ social support systems and subsequent impacts on mental health symptoms and suicide risk.
- Johanna Eliacin (Indianapolis, Indiana): Expanding VA Peer Support Workforce Capacity to Facilitate Increased Access to VHA Mental Health Services and Continuity of Care for Veterans with Mental Illness During the COVID-19 Pandemic. Leveraging the Principal Investigator’s ongoing Career Development Award project, this qualitative study seeks to understand impacts of the COVID-19 pandemic on delivery and adaptations for peer support programs in mental health, including successful strategies for enhancing peer support to improve Veterans’ access to care.
- Angela Fagerlin (Salt Lake City, Utah): Veterans’ Experiences During the COVID-19 Pandemic. This short-term longitudinal study leverages the existing infrastructure of an ongoing COVID-19 study to identify challenges and facilitators to physical distancing; understand access to VA and non-VA medical care; and assess impacts of social isolation on loneliness and emotional coping.
- Jennifer Funderburk and Robyn Shepardson (Syracuse, New York): Piloting a Self-Help Intervention to Improve Veteran Mental Health During the COVID-19 Pandemic. This mixed methods study assesses the effects of the Managing Emotions in Disaster and Crisis (MEDIC) intervention on psychological distress, depressive symptoms, anxiety symptoms, social connectedness, and overall well-being, along with implementation strategies and outcomes.
- Bo Kim (Boston, Massachusetts): Applying the After Action Review Methodology to Examine Mental Health Residential Rehabilitation and Treatment Programs’ (RRTP) Response to the COVID-19 Crisis. Using qualitative methods, this study explores challenges, adaptations, and performance of RRTPs in their initial response to the pandemic, and how that might inform subsequent response strategies.
- Diana Mendez (Orlando, Florida): Changes in the Delivery of Evidence-Based Psychotherapies for Depression and PTSD as a Result of the COVID-19 Pandemic. Using secondary analyses of data from ongoing research, the study team is assessing impacts of the sudden shift to telehealth strategies on treatment utilization (frequency and duration) and mental health outcomes (prescription changes, Veterans Crisis Line calls, chart flagging for suicide).
- Lisa Silbert (Portland, Oregon): Impact of Social Distancing During the COVID-19 Pandemic on Cognitive, Physical, and Mental Health in Urban and Rural Veterans in the Pacific Northwest. Leveraging data and infrastructure from an ongoing study of the VA Clinical Assessment, Reporting and Tracking Program, investigators are assessing the impact of COVID-19 pandemic distancing restrictions on social activities (overnight visitors and travel), digital biomarkers (step counts, sleep duration, time in/out of the house), psychological distress, and physical illness.
- Alan Teo (Portland, Oregon): Adapting Caring Contacts to Counteract Adverse Effects of Social Distancing Among High-Risk Veterans During the COVID-19 Pandemic. This project is planning for a large randomized clinical trial by involving an expert panel to (1) develop an adapted version of the Caring Contacts intervention (“Crisis Caring Contacts”), and (2) construct a cohort and develop data collection instruments and protocols.
Understanding and mitigating the adverse mental health impacts of the COVID-19 pandemic among Veterans is a priority for VA. The current research funded by HSR&D, including, but not limited to, the Rapid Response projects, as well as other studies supported by the Office of Research and Development (ORD), are addressing multiple aspects of the potential relationships between the COVID-19 pandemic and clinical and behavioral health outcomes. Still, much work remains to be done in addressing important evidence gaps, including identifying vulnerable groups most at risk for adverse mental health outcomes; understanding the underlying mechanisms (e.g., social, economic, and public health prevention factors); and examining facilitators and barriers to accessing effective and timely treatment for mental health conditions. HSR&D is working across ORD and with our program partners to address these challenges and to support continued, coordinated, and Veteran-centric studies that will improve the quality of mental healthcare for Veterans during and after the COVID-19 pandemic.
- Panchal N, Kamal R, Cox R, and Garfield R (2021). The Implications of COVID-19 for Mental Health and Substance Use. Kaiser Family Foundation. Available at: https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/.
- McNutt, Marcia. “The Coronavirus Pandemic: Delivering Science in a Crisis.” Issues in Science and Technology (June 16, 2020). Available at: https://issues.org/ mcnutt-actionable-strategic-irreplaceable-data-deliver-ing-science-in-a-crisis/
|