
|
|
Response to CommentaryThe Role of Research and Evaluation in Addressing VHA Employee Burnout and Well-beingVHA has paid increasing attention to burnout and well-being, particularly among clinicians, and those efforts have become more salient during the global COVID-19 pandemic. Since 2013, VHA has collected information on burnout in its annual All Employee Survey (AES). In 2017, VHA hosted a Physician Burnout Research Summit to assess what we know and identify what we still need to learn about the scope, drivers, and outcomes of VHA physician burnout. Since then, VHA efforts to address burnout have expanded in multiple ways. Established in 2020, the VHA Employee Engagement and Workforce Stability Research Group (VEEWS) serves as a forum for VHA researchers and operational partners to generate ideas, methods, and meaningful organizational change to address employee burnout and well-being. VEEWS also serves as a space for VHA researchers and operational partners to discuss ongoing VHA efforts, and review research and evaluation findings. Since its inception, VEEWS has worked with several VHA operational partners, including the Office of Academic Affiliations and the Office of Patient Centered Care and Cultural Transformation to identify key strategic priority areas. Recently, VHA’s Health Services Research and Development (HSR&D) Service partnered with AcademyHealth, the leading health services research and policy organization, to convene a VHA Clinician Burnout Advisory Group tasked with developing a research agenda to address burnout at VHA. The advisory group will align with the Reduce Employee Burnout and Optimize Organizational Thriving (REBOOT) task force, described in this issue’s commentary article. Also, this year HSR&D solicited applications for Researchers and Evaluators in Residence (REiR) to help provide initial evaluation support for pilot programs selected by the REBOOT task force. Insights from these efforts will inform large- scale evaluations examining the impact of these pilot programs and the potential for systemwide scalability. VHA must now employ evidence-based approaches toward targeted interventions that address clinician burnout and well-being, while expanding its efforts to better understand the experiences of non-clinician employees. Clinician Burnout within VHAMultiple research and operations-funded efforts to understand burnout and employee well-being are underway. We lead two existing HSR&D funded investigator-initiated research (IIR) studies on burnout within VHA (ESW: IIR 15-363; KZ: IIR 17-262). Our work focuses on primary care physicians and mental health clinicians (i.e., psychiatrists, psychologists, and social workers), the two clinical specialties with the highest reported levels of burnout among VHA providers.1 We have found clear evidence that workload represents the leading driver of burnout.2,3 We have less clarity on how to address this organization-level challenge, how to decrease workload to reduce burnout, increase thriving, and improve employee well-being and Veteran outcomes. However, prior VHA research suggests that inadequate staffing explains part of the adverse effect of workload.4 Although the AES asks respondents to rate their level of burnout, it does not ask about factors contributing to their burnout. A follow-up AES question asks whether respondents plan to leave VA within the next year (i.e., turnover intention), and “what is the primary factor that has led you to consider leaving your current position?” Responses to this question require further exploration and might reveal preferred ways in which VHA could address clinician (and overall employee) needs, such as compensation and/ or benefits realignment, as well as flexible work arrangements (e.g., telework, alternative work schedules) that could improve workload or otherwise influence employee experience. Further, AES could incorporate items measuring employee well-being used in other health systems. As REBOOT pivots toward organizational interventions designed to address burnout and employee well-being, these interventions must be evidence-based, actionable, and locally supported. To maintain the momentum of current efforts, those designing and implementing interventions must consider existing employee burnout and employee bandwidth to adopt interventions aimed at addressing their burnout and improving their well-being. A VHA Research and Evaluation AgendaAs a learning health system, VHA can take several steps to ensure the long-term success of programs such as REBOOT. First, VHA needs better metrics that link employee experiences to behaviors and outcomes. For example, if one of the pilot interventions involves changing training requirements, we must arrive at a consensus on how to measure requirements, how they change, and the impact of the change on employees. Ideally, we would conduct randomized interventions or implement stepped wedge designs if randomization proves infeasible and assess the impact of interventions over time using both subjective and objective measures of employee burnout and well-being. We must standardize the collection, tracking, and updating of key employee metrics (e.g., date of hire, transitions within VHA between services, tenure in each role, burnout from AES, well-being). We must make metrics available to managers, leadership, a better understanding of what it entails, and greater confidence and willingness to recommend similar activities to patients. Employees also noted the importance of supervisors and medical center directors who send clear and positive messages that support employees’ participation in EWH. In fact, a recent pilot study led by OPCC&CT has started to examine the effect of allowing 30 minutes per week of dedicated time for EWH. Further, those who participated in EWH activities reported feeling less stressed and reported that they felt a greater ability to deal with difficult situations on the job. One individual reported that mindfulness practices would better prepare her to engage in difficult conversations with family members of Veterans. To support EWH, clear VA policies and guidance would help encourage and support employees in taking time to participate in EWH activities. Such an effort may lead to a more refreshed and focused employee workforce, an important issue given the staff retention challenges that VA and other health care systems are currently experiencing. 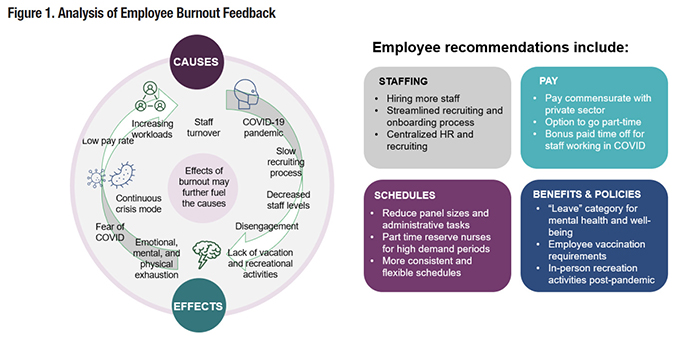
References
|
|