
|
|
CommentaryPrecision Oncology at VA: Clinical Applications for a Learning Healthcare SystemVA takes care of approximately 450,000 patients every year who are on the cancer care continuum – from screening to survivorship. There are about 43,000 new cancer diagnoses every year in VA, and approximately 25 percent are rare cancers. VA is leading the fight against cancer through precision oncology approaches that are informed and reinforced by new discoveries from cancer research. This fusion of clinical treatment and research is the cornerstone of the care VA provides Veterans undergoing cancer treatment. VA actively leverages treatment discovery and clinical development by collecting population-wide data on cancer recurrences and metastatic cancer development – accomplished by the cancer registry data that underpins programmatic decisions within cancer care. By linking these data points to individual characteristics of patients and their tumors, treatments, and clinical outcomes, VA is building systemic, comprehensive data tools that support both clinical needs and research priorities. Cancer is a genomic disease, and it has been firmly established that inherited and acquired genetic variations have a profound impact on the effectiveness of different anti-cancer drugs. As such, the use of precision oncology approaches in the treatment of our Veterans is essential. The National Precision Oncology Program (NPOP) was created in response to the 2016 Cancer Moonshot call to action. Since the program launched, more than 34,000 Veterans, most with advanced cancer, have had their care guided by molecular testing, and more than 50,000 molecular tests have been ordered. Having expanded from just one cancer type – metastatic lung cancer – to lung cancers, pancreatic cancers, and advanced cholangiocarcinoma, bladder, other advanced solid tumors and all rare cancers, NPOP has evolved into a program that equips providers with the right treatment for the right Veteran, at the right time. NPOP then uses its molecular testing database in novel clinical decision support tools that aid in Veteran treatment decisions, help families understand potential risks for developing certain cancers, determine program operational needs, and that inform research. NPOP is one of the few programs in the nation that routinely screens cancer patients for genomic and proteomic abnormalities to align targeted therapies to tumor type. Further, when new clinical guidelines or therapies enter the scientific body of knowledge, NPOP re-analyzes the current database of Veterans to identify if new therapies or approaches have become available. From there, clinicians can evaluate if treatment approaches need to be adjusted. Veterans are uniquely able to access genomic testing without the financial burden that may be experienced by their civilian peers. Precision oncology generates vast amounts of complex genomic and molecular data that clinicians must interpret and apply to patient care. This requires a high level of expertise in molecular biology and genomics, as well as specialized bioinformatics tools to help analyze the data. VA clinicians must also communicate the significance of this data to patients in a way that is easily understandable, keeping in mind that Veterans often have dynamic social environments with family members and caregivers intimately engaged in the cancer journey. Improved accuracy of genomic profiling helps clinicians identify the most appropriate treatment options for individual patients. That is why clinical treatment of cancer is increasingly driven by precision oncology approaches – and has moved from treatments based on type and histology alone to treatment decisions based on patient-specific molecular characteristics including protein expression and comprehensive genomic profiling. Precision oncology can also help identify environmental exposures that may have contributed to a Veteran’s cancer diagnosis. For example, some patterns of genetic mutations may be linked to exposure to carcinogens such as Agent Orange or radiation. Identifying these environmental exposures can help clinicians develop more targeted treatment plans and prevent future exposures. One such effort is the Molecular Analysis Researching Carcinogenic Exposures research project (MARCE), which is focused on a cohort of tumor samples from Veterans who were stationed at Marine Corps Base Camp Lejeune between 1950 and 1985. Researchers are looking to understand and identify the impact that contaminated drinking water may have had on the pattern of DNA mutations that occur in tumors linked to exposure to the drinking water contaminants, including cancers of the kidney, multiple myeloma, bladder, liver, leukemia (bone marrow), and others. This specific research effort is geared towards further understanding the effects of military environmental exposures, and their clinical implications. As seen with MARCE, precision oncology generates new questions and challenges for cancer researchers. As precision oncology approaches become more widespread, and researchers continue to explore new targets for therapy, our community of clinician-scientists must work to expand and refine biomarkers that predict response to treatment and develop strategies to overcome resistance to treatment. We must also develop new technologies and tools for analyzing the complex molecular and genetic data that is generated by precision oncology. Overall, precision oncology and cancer research are mutually reinforcing fields that depend on each other for progress. Precision oncology relies on the findings of cancer research to develop new therapies, while cancer research depends on precision oncology to validate new discoveries and successfully translate them into clinical practice. This symbiotic approach embodies the learning healthcare model that VA strives towards, all while centering on the needs of the Veteran. 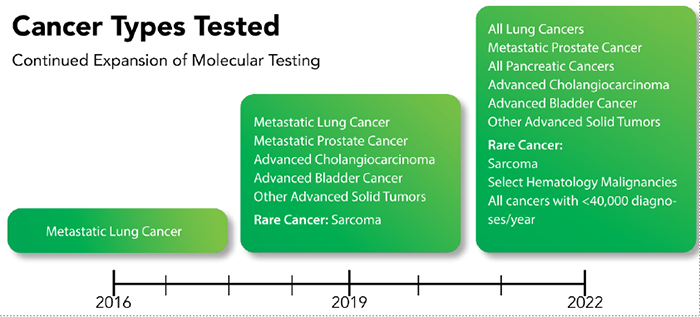
|
|
Next ❯