
|
|
Response to CommentaryCenter Crosses Boundaries to Promote Better Care for Aging VeteransAs highlighted in Dr. Shaughnessy’s commentary, the Office of Geriatrics and Extended Care (GEC) provides a wide array of services to meet the needs of Veterans with functional limitations from aging, disability, and disease. The breadth of GEC programming and the heterogeneity of Veterans served creates many opportunities for research. Most importantly, the VA system has a support infrastructure that facilitates asking (and answering) critical questions that otherwise could not be considered. VA’s geriatric service has always emphasized managing complex Veterans with multimorbidity, cognitive impairments, and functional deficits. However, the older Veteran population is changing. With the aging of Vietnam Veterans, there is an increased prevalence of serious mental illness, which is superimposed onto the existing complexities of aging. This trend is occurring in the context of fewer social supports for the older Veteran population, and creates challenges for traditional GEC programs. This shift also creates opportunities to develop, test, and implement innovative modifications that meet the needs of Veterans and their caregivers. Veterans have been clear on one aspect of care; they prefer to remain at home, if possible. To support this, Congress included the suite of VA created home and community based services (HCBS) in the Millennium Act of 1999. However, a recent VA Evidence Synthesis Program systematic review found that only a handful of high quality studies exists that demonstrate the ability of HCBS to prevent or delay nursing home placement. As the MISSION Act expands support for Veterans and caregivers in the community, there is substantial opportunity to improve the evidence base supporting HCBS in VA, as well as identifying the Veterans who would most benefit. When Veterans are unable to reside in the community, facility-based care (long term care) provides necessary home support as well as medical support, activities, and socialization. VA provides or purchases more than 7 million bed days of care in community nursing homes and is projecting a 25 percent increase in the next decade. The nursing facility setting has unique challenges inside and outside of VA. These facilities serve a highly vulnerable population, are under significant financial pressure, and experience a high degree of staff turnover; all these factors greatly complicate the delivery of quality care to aging Veterans. Community nursing homes are highly regulated, with mandatory inspections, reporting, and oversight. In addition, data on patients’ experiences in Community Living Centers and VA purchased Community Nursing Homes are summarized in a publicly reported quality report, which is available on www.AccessToCare.va.gov. As a large purchaser of facility-based care, VA is in a unique position to negotiate care based on proximity, quality, and cost. Working in collaboration with GEC, the HSR&D-funded Center of Innovation in Long Term Services (COIN-LTSS) has built a research portfolio focused on helping Veterans overcome the challenges of age, disability, and disease. In addition to the LTSS research portfolio, the COIN-LTSS has built relationships with programs focused on older Veterans with multimorbidity, homelessness, food insecurity, and suicide risk. The center has completed research projects focused on HCBS, including collaborations with the Veterans Benefit Administration. More recently, the COIN-LTSS has collaborated with the Veteran Experience Center to provide data support with the VA Choose Home initiative. To support this infrastructure, we have close collaborators in the GEC Data and Analysis Center. The investigators within the COIN-LTSS have a particular expertise in pragmatic trials in nursing homes. The COIN-LTSS served as home to the Long Term Care CREATE, which included a pragmatic trial of the INTERACT intervention. The LTC CREATE included development data on the Bright Spots program and Medical Foster Home; these data have subsequently been utilized by our GEC colleagues to advocate for operationalization of the programs. Another LTC CREATE project, Community Discharge, led to the development of a CMS NH Compare measure. Investigators within the COIN-LTSS are internationally recognized for antimicrobial stewardship within the nursing facility including measurement of antibiotic resistance, procedures to improve adherence to the evidence base, and improving vaccination outcomes. GEC and the COIN-LTSS are participating organizations in the Embedded Pragmatic Alzheimer’s Disease Clinical Trials Collaboratory, an NIA-funded initiative that brings together research, industry, and VA with a focus on pragmatic trials in nursing facilities. Brown University School of Public Health recently completed one such pragmatic trial, randomizing nursing homes to high dose vs. regular dose influenza vaccination. Importantly, this trial was a win-win-win: nursing facilities received discounted influenza vaccine, residents were vaccinated at higher rates, staff received workplace vaccinations, and the study generated knowledge of the value of high dose influenza vaccination to protect nursing facility residents from influenza and its associated outcomes. The trial utilized existing nursing home data and claims to analyze resident level outcomes. The COIN-LTSS is a unique place for research—it provides a base for those with a passion for caring for functionally impaired Veterans. COIN-LTSS researchers are uniquely skilled in the measurement of LTSS outcomes, and have a strong history of working together to implement change. 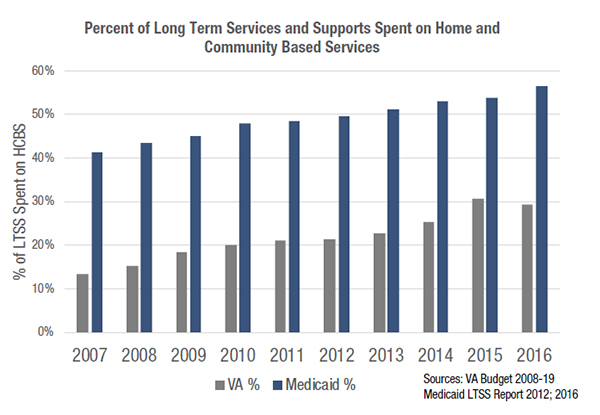
|
|