
|
|
Research HighlightThe Role of Telehealth in Increasing Treatment Utilization Among Veterans with Substance Use DisordersKey Points
Overdose mortality continues to rise in the United States, but major shifts have occurred in who is at highest risk. In recent years, rapid increases in opioid-involved overdose have been driven by heroin and synthetic opioids. However, less recognized are the major increases in morbidity and mortality related to other substances and use of multiple substances. More than 60 percent of opioid overdoses now involve at least one other substance and many involve multiple other substances, with major increases in overdoses related to methamphetamine and cocaine.1 Simultaneously, mortality related to alcohol use has increased and is implicated in the deaths of more than 95,000 people annually.2 We now see that the overdose epidemic is really an epidemic of the impacts from substance use and other comorbid medical conditions. Thus, it is critical that the Veterans Health Administration (VHA) continues to lead national efforts to address the impacts of substance use in the Veteran population. Substance use disorders (SUDs) remain the common denominator and major risk factor for overdose even as trends have shiftedin the type and combination of substances. Yet, despite such extensive negative impacts from SUDs, treatment rates remain low and are much lower than other mental health conditions. In 2019, 6 percent of Veterans had an SUD, an increase over prior years, but 85 percent of these Veterans did not receive any treatment for their SUD.3 Key barriers to SUD care include stigma (at the societal, healthcare system, and patient levels), the underlying complex symptoms of addiction, and limited accessibility of treatment. Limited accessibility, including both a limited number of clinicians and clinics, and long distances to care, is an under-recognized and modifiable barrier for SUD treatment. Distance to care is especially relevant for SUD care, which typically requires frequent visits over a long period of time in a patient population that often has limited transportation, childcare, and other psychosocial resources. VHA has been a national leader in developing, testing, and implementing telehealth interventions to improve access to care. Across decades of research, telehealth- delivered treatments have been shown to be non-inferior to in-person treatment, including for mental health conditions. In addition, there are indications that telehealth can potentially reduce barriers to care, including stigma and accessibility. However, to date, there have been very few studies on the use of telehealth for treatment of SUDs, including in VHA. The COVID-19 pandemic has prompted a rapid and unprecedented expansion of telehealth across health conditions. Specifically for SUD care, changes in national regulations and state guidance have decreased barriers and enhanced support for the use of telehealth in delivering SUD care.4 These changes were specifically to support social distancing and healthcare operations during the pandemic. Additional data is needed to help inform whether these policies should persist, particularly those impacting essential care for SUDs. Thus, this proves to be a critical time to better understand which patients benefit from telehealth, the impacts of telehealth on both patients and clinicians, and ongoing barriers to SUD care. Below, we describe three ongoing projects aimed at understanding the impacts of telehealth and at informing how to harness fully the potential of telehealth for improved SUD care in the future. First, to better understand patient experiences using telehealth for SUD treatment, we completed semi-structured qualitative interviews of Veterans with opioid or alcohol use disorders. We conducted the vast majority of interviews after the start of COVID-19. The goals of these interviews were to elucidate design characteristics of telehealth SUD treatment, perceptions of telehealth for SUD treatment, and barriers and facilitators to SUD telehealth care. Our findings demonstrate the wide range of Veteran views and experiences, which depend on patient-specific factors including living environment, comfort with technology, experiences with in-person care, resources, and feasibility of treatment alternatives. Table 1 highlights some of the key themes categorized as potential telehealth advantages, disadvantages, and ongoing considerations to improve the care experience. Many patients discussed the increased ease and accessibility of treatment they had received via telehealth, which had allowed them to fit ongoing treatment into their busy schedules, saving time and money in travel costs, and providing the ability to discuss sensitive topics in the privacy and comfort of their own homes. However, some Veterans mentioned drawbacks related to personal preference. These Veterans stated that the use of technology “doesn’t feel the same,” and found value in leaving their home for care. We also identified several ongoing barriers to care, including limited access to the internet and lack of privacy at home, which posed a specific barrier to videoconferencing. Our findings highlight the critical importance of telehealth for those Veterans who have minimal access to in-person specialty SUD care, but also the importance of the option of telehealth for the broader population of Veterans to help decrease stigma and increase accessibility to SUD care. Second, in response to increased rates of opioid use disorder (OUD) and opioid-related overdose in the Veteran population, increasing access to OUD pharmacotherapy, specifically to the medication buprenorphine, is a key VHA priority. This priority underscores the need for a better understanding of the impact of telehealth for OUD treatment on patient outcomes. We recently examined VHA’s innovative use of telehealth for buprenorphine treatment pre-COVID-195 and are currently evaluating impacts from the dramatic increase in telehealth (both phone and video) for buprenorphine treatment on patient outcomes and disparities in care since the start of COVID-19. In many ways, VHA has led the nation in implementing telehealth, and this provides a critical window to examining impacts of this investment on the vulnerable SUD patient population. Third, a critical barrier to access to OUD treatment is limited capacity because of a lack of trained buprenorphine providers at many VHA facilities. Prior work has identified patient- level demographic and clinical factors that contribute to low buprenorphine treatment. However, we have little understanding of clinician-level factors, which are a key driver of care delivery. To better understand this, we are currently disseminating a survey across VHA assessing buprenorphine prescriber attitudes and practices initiating and continuing buprenorphine for Veterans with OUD, including via telehealth. Prior to COVID-19, some clinics were beginning to use telehealth for SUD care but only in limited ways. In contrast, since the start of COVID-19, care has transformed so that telehealth is now the default mode for providing care. Next, we must determine the future role of telehealth and how can it be used to support high-quality patient-centered SUD care in a post-COVID world. Our recent work emphasized the importance of choice for all Veterans and acknowledged that feasible treatment alternatives vary for each Veteran; there are likely some Veterans for whom in-person care is preferred and others for whom telehealth is not only more effective, but may actually increase access to needed treatments that were previously not accessible. In addition, to truly harness the potential of telehealth to increase care for the 85 percent not in SUD treatment, we must develop new models of care that can help engage patients and deliver more patient- centered and accessible care. 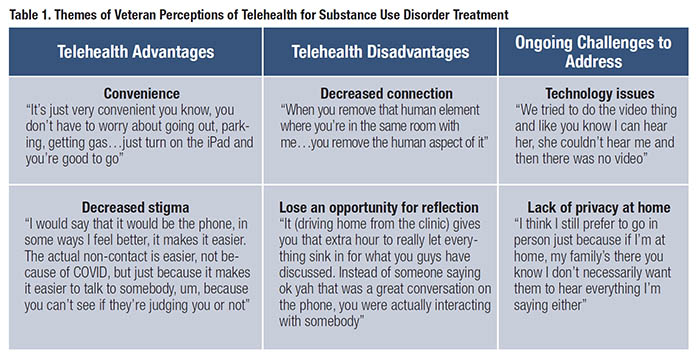
References
|
|