
|
|
Innovation UpdateSelf-Help Crisis Intervention to Improve Mental Health Among At-Risk Veterans During the COVID-19 PandemicMany Veterans report symptoms meeting criteria for psychiatric disorders, such as Major Depressive Disorder (MDD) and Posttraumatic Stress Disorder (PTSD), but are not engaged in mental health treatment. Stressful events, such as the COVID-19 pandemic or natural disasters, often exacerbate mental health symptoms, leading to increased impairment and suicide risk. Unfortunately, there is a dearth of evidence-based strategies that primary care teams can offer to support patients during these stressful events. Thus, in response to the COVID-19 pandemic, we developed a self-help crisis intervention called Managing Emotions in Disaster and Crisis (MEDIC) that aims to improve mental health among at-risk Veterans. Delivered via mail or email, MEDIC provides two evidence-based, cognitive-behavioral, self-management strategies on a weekly basis over the course of four weeks (see Figure 1). Veterans may also choose brief individual support calls with a Primary Care-Mental Health Integration (PC-MHI) provider or group telephone support calls with a peer. To test the effectiveness of MEDIC in an open trial, we recruited 117 Veterans in late 2020 who were either living in rural areas (~75 percent) or participating in VA’s Veteran Integration to Academic Leadership (VITAL) program (~25 percent), and who were not engaged in psychotherapy but had current MDD or PTSD symptoms. We collected post data (n=108) at six weeks and follow-up data (n=62) at six months. Findings: Results provide preliminary support for the acceptability and effectiveness of MEDIC.
Implications: Although further research is needed, MEDIC shows great promise as a self-help intervention to support at-risk Veterans’ mental health during crises and disasters. Its low-intensity format (<1 provider hour required per Veteran across four weeks) enhances feasibility for busy primary care clinics. 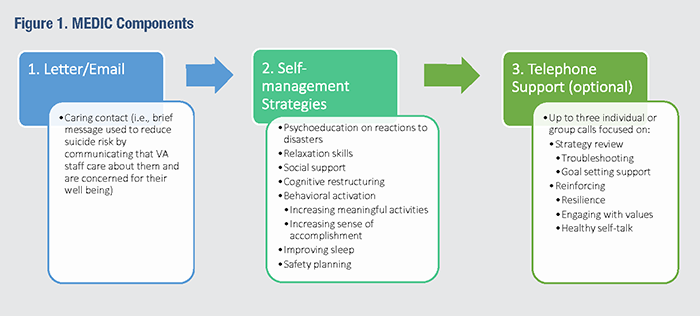
|
|
❮ Previous |