
|
|
Research HighlightGeographic, Patient, and VA Medical Center Variation in Receipt of Primary Care in a National Sample of Veterans with DiabetesKey Findings
During the pandemic, patients with chronic disease were more likely to miss primary care medical appointments when compared to pre-pandemic times (Wong SYS, et al., 2020). Guidance on confinement to reduce the risk of COVID-19 among vulnerable patient populations contradicted usual recommendations to maintain a regular patient-provider relationship in order to ensure care coordination for medications, education, and laboratory monitoring (Beran, et al., 2021). Concerns about the lack of continuity of care during the pandemic persist among clinicians, and the downstream effects of disruptions in care on disease management are still unknown (Verhoeven, Tsakidzitis, Philips, & Van Royen, 2020). As part of an HSR&D-funded Rapid Response Project, we examined the geographic, patient, and VA medical center characteristics among a cohort of Veterans with Type 2 diabetes receiving primary care in the VA healthcare system. VA is the nation’s largest provider of telehealth, with telemedicine infrastructure in place before the onset of the pandemic; community ordinances and closures during the pandemic required VA to expand this infrastructure. By considering demographics, disease burden, VA medical center characteristics, social vulnerability, and regional effects, we addressed social determinants in COVID-19 research and produced an analysis of primary care during one point in the pandemic. ResultsOur final cohort consisted of 1.6 million Veterans with Type 2 diabetes residing in 125 VA medical center catchment areas who received primary care in VA in FY 2018 or 2019, of whom 73 percent were non-Hispanic White (NHW), 22 percent were non-Hispanic Black (NHB), and 6 percent were Hispanic. The mean age was 70 years and 95 percent were male. We adjusted all analyses for age, gender, race, rural-urban residence, service-connected disability, marital status, the van Walraven comorbidity score, diabetes medication use and type, diabetes control prior to the pandemic, quartile of the CDC social vulnerability index, pre-pandemic VA medical center, telehealth adoption, and spatial random effects for catchment areas. Figure 1 provides a probability map of having a primary care visit by catchment area for the study population based on parameter estimates with shading reflecting adjusted quintile of probability estimates. Results from our adjusted logistic regression analysis revealed that the prevalence of having any primary care visit during the 4th quarter of 2020 varied substantially by VA medical center catchment area with values ranging from 22 percent to 60 percent. The legend reflects the catchment areas with the highest and lowest probability of receiving any primary care within each quintile. The odds of having any type of primary care visit decreased slightly with increasing age and were lower in men than women. Relative to NHW, the odds of having any type of primary care visit were similar in NHB and Hispanics. The odds of having any type of primary care visit were also similar in rural and urban Veterans and in married compared to non-married Veterans. Having a service-connected disability of at least 50 percent was associated with higher odds of having any type of primary care visit as was use of diabetes medication, while pre-pandemic Hemoglobin A1c levels were inversely associated with the odds of having any type of primary care visit. We found that Veterans living in areas with the highest socially vulnerable index were more likely to have any type of primary care visit than Veterans living in areas with the lowest social vulnerability. With respect to pre-pandemic telehealth acuity, Veterans at VA medical centers with lower levels of telehealth prior to the pandemic were 40 percent less likely to have any type of primary care visit during the 4th quarter of 2020 than Veterans at VA medical centers with higher levels of telehealth adoption prior to the pandemic. ConclusionIn this study, we sought to examine geographic, patient-level, and VA-medical center variation in the receipt of primary care during the COVID-19 pandemic. Our cohort of Veterans with Type 2 diabetes receiving care in VA presented a unique opportunity to study a vulnerable population within a healthcare system that had existing infrastructure to deliver telemedicine during an unprecedented global pandemic. In our first analysis, we modeled the receipt of any primary care in the fourth quarter of fiscal year 2020. We observed that even after covariate adjustment accounting for patient and VA medical center factors, substantial spatial variation in receipt of primary care remained. This result indicates that there were other geographically varying factors that were associated with primary care receipt during the pandemic. Regional variation in COVID-19 burden and local ordinances and closures could explain part of the unaccounted variability. In this same analysis, we observed that as social vulnerability increased, the probability of receiving primary care also increased. This result indicates that patients living in areas characterized by socioeconomic, housing, and transportation vulnerability were more likely to receive primary care than their peers living in areas without these risk factors. These patients may disproportionately rely on community care and services that shut down during the pandemic, requiring them to utilize VA resources more heavily; however, our study is limited to VA services only and does not currently look at care received outside VA. Additionally, we found that lower pre-pandemic VA medical center telehealth acuity was associated with a lower overall probability of receiving primary care during the pandemic. One possible explanation is that areas with lower rates of telehealth utilization pre-pandemic were also “underprepared” to manage care in the event of a public health emergency even after adjusting for the social vulnerability of patients in the area. Recent studies suggest that patients prefer in-person visits (Predmore, Roth, Breslau, Fischer, & Uscher-Pines, 2021), so understanding the barriers to access will be important going forward. Lastly, translating the differences we observed in primary care during the pandemic to patient health outcomes such as hospitalization and mortality will direct the next phases of research so that they offer guidance to the medical community. 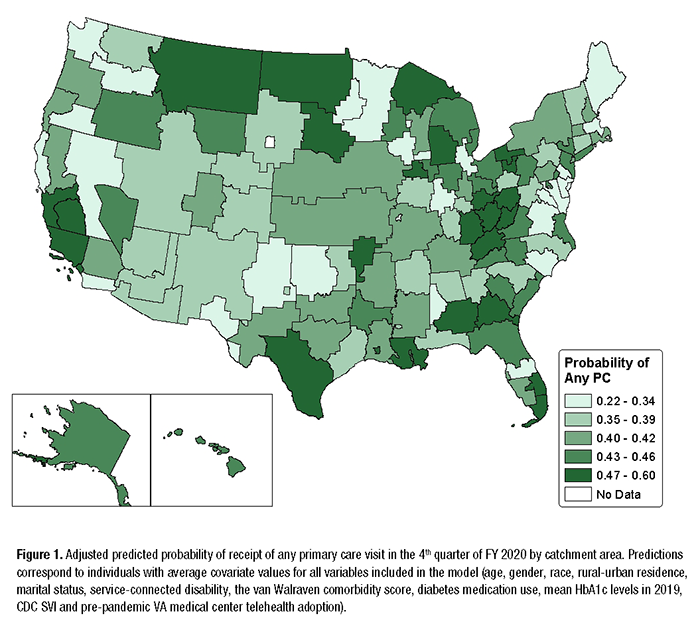
References
|
|