 |
Making an IMPaCT in our Communities: Community Health Workers Improve Healthcare for High-Risk VeteransHSR&D’s monthly publication Veterans’ Perspectives highlights research conducted by HSR&D and/or QUERI investigators, showcasing the importance of research for Veterans – and the importance of Veterans for research. In the February 2019 Issue:Individualized Management for Patient-Centered Targets (IMPaCT) Program |
What is IMPaCT?The Individualized Management for Patient-Centered Targets (IMPaCT) Program is a standardized, scalable, and evidence-based model of care.In the IMPaCT model, Community Health Workers (CHW) join care teams and help patients navigate the healthcare system and connect to resources. IntroductionEvery day, Veterans struggle with real-life challenges such as hunger, housing insecurity, and trauma. These unmet social needs contribute to known health disparities: Veterans have higher rates of chronic illnesses such as diabetes, heart disease, and hypertension (72% compared to 40% of other U.S. adults), and up to a 14-fold higher risk of mental health issues such as post-traumatic stress disorder (PTSD). To address these issues, the Corporal Michael J. Crescenz VA Medical Center (CMCVA) in Philadelphia invested in a new and unique workforce—Community Health Workers (CHW). CHWs are trusted laypeople who share a common background – race, income, Veteran status – with their patients. While CHWs are well-positioned to build trust with fellow Veterans and address unmet social needs, to date they have not been widely deployed within the VA healthcare system. Center for Health Equity Research and PromotionHSR&D's Center for Health Equity Research and Promotion (CHERP) represents a well-established collaboration between the VA Pittsburgh Healthcare System and Corporal Michael J. Crescenz VA Medical Center in Philadelphia and their respective academic affiliates, the University of Pittsburgh and University of Pennsylvania. CHERP's mission is to advance the quality and equity of health and healthcare for Veterans, especially those from vulnerable populations.Partnerships Improving Community CareTo ensure the CHW program was effective, the CMCVA looked to its neighbor – the University of Pennsylvania Health System – for guidance. Dr. Shreya Kangovi, a Penn primary care physician and researcher, designed and tested IMPaCT (Individualized Management for Patient-Centered Targets), which is a standardized, scalable, and evidence-based model of care. In the IMPaCT model, CHWs join care teams and help patients navigate the healthcare system and connect to resources. They also do things that busy doctors, nurses, and social workers cannot: exercising together with patients at the local gym or shopping for produce and cooking a healthy meal together. In 2014, CMCVA started using IMPaCT CHWs to support high-risk Veterans. Veterans Helping Each Other: A Healing GardenOne Veteran connected to the program, who we’ll call Mr. Jones to protect his privacy, was struggling with depression brought on by the challenges of finding steady employment given his incarceration history. When Mr. Jones met Anthony Davis, a fellow Veteran and CMCVA CHW, the two men bonded over their experience in the military and having grown up in the same area of West Philadelphia. Mr. Jones felt comfortable opening up to Mr. Davis, telling him how he spent most of his time alone in his house, smoking cigarettes. 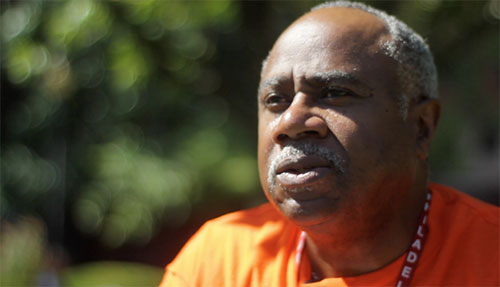
Anthony Davis, Community Health Worker and part of IMPaCT. Mr. Davis, who noticed that a lot of his patients were struggling with depression and PTSD, started a weekly gathering with socially isolated Veterans and invited Mr. Jones. “I took my time with each of my patients and got them to come out each week to social activities like movies or bowling,” said Mr. Davis. “We even planted an urban garden – you can see the difference in their personalities.” 
Veterans tend an urban garden as part of the IMPaCT program. As a result of Mr. Jones’s participation in these activities, and with Mr. Davis’s support in finding steady employment, he’s cut down on his smoking and says he feels happier. “My mission is to bring people together,” Mr. Davis says. “As a team, we help to guide them and give them back their independence.” “My mission is to bring people together,” Mr. Davis says. “As a team, we help to guide them and give them back their independence.” - Anthony Davis, Community Health WorkerPositive Effects of Peer SupportJudith A. Long, MD, Co-Director of HSR&D’s Center for Health Equity Research & Promotion (CHERP) in Philadelphia, has observed low-income Veterans’ need for a different kind of support during her two decades as a VA physician. She has led numerous research studies on the positive effects of peer support on outcomes for vulnerable populations. Dr. Long also translated results to implementation when she brought the IMPaCT model to CMCVA. “1.5 million Veterans live in poverty and face social challenges that make it hard for them to stay healthy,” says Dr. Long. “For Veterans dealing with serious real-life problems, such as chronic medical conditions, hunger, and poor housing, community health workers do a great job of building trust and helping to address pressing, unmet needs,” says Long. “IMPaCT effectively addresses many of the problems that we struggle with in VA: dealing with complex social and behavioral needs, improving chronic disease control, increasing access to care, and lowering costs.” IMPaCT Addresses Many Problems“IMPaCT effectively addresses many of the problems that we struggle with in VA: dealing with complex social and behavioral needs, improving chronic disease control, increasing access to care, and lowering costs.”IMPaCT’s one-on-one peer support, reinforced by standardized elements including hiring algorithms, training, supervision, and clinical integration guidelines, has paid off. Tested in three randomized controlled trials, the model has shown consistent improvements in chronic disease control, mental health, quality, and primary care access, while reducing costly hospitalizations. The latest multi-site trial included the CMCVA and demonstrated a two-fold increase in patient satisfaction and a 65% reduction in hospital days.1 Both Penn Medicine and CMCVA have adopted IMPaCT as part of their system-wide population health management strategies for high-risk patients and have served more than 8,000 people in Philadelphia. Expanding the IMPaCT ProgramIMPaCT Implementation"It only takes six months to get an IMPaCT program – capable of serving 2,000 patients a year-up and running within a VA Medical Center," says Dr. Long.As team leader for “Better Health, Lower Cost: How IMPaCT Community Health Workers Can Support Veterans,” Dr. Long was awarded Gold Status in the 2018 VA Shark Tank Competition, which identifies field-developed promising practices and facilitates the dissemination of those practices across the VA healthcare system. The IMPaCT model will be implemented in two more VA facilities starting this spring, with the potential to expand to more facilities across the country. “It only takes six months to get an IMPaCT program – capable of serving 2,000 patients a year –up and running within a VA Medical Center,” says Dr. Long. “The cost of the program is $1,250 per patient, including salaries, supplies, and training. There’s a 2:1 return within the fiscal year for the investment. Most importantly, vulnerable Veterans receive care and have much better health.” For more information about IMPaCT, please contact Dr. Judith Long at Judith.Long@va.gov .
|