 |
Helping Homeless Veterans Cross the Digital Divide for Increased Access to HealthcareVeterans’ Perspectives highlights research conducted by HSR&D and/or QUERI investigators, showcasing the importance of research for Veterans – and the importance of Veterans for research. In the May-June 2023 Issue:
|
Introduction
"We had Veterans' input at every phase of intervention development" in this study, says lead investigator Lynn Garvin, PhD, MBA, "which increases the likelihood of connecting Veterans experiencing homelessness and substance use disorder with VA virtual care, the modality they prefer."
Veterans experiencing homelessness have elevated rates of mental illness 1 and substance use disorder (SUD), 2 and twice the rate of fatal overdose as the general population. 3 Homelessness compounded by SUD increases health risks—often with fatal consequences—making it imperative to connect Veterans experiencing homelessness and SUD to healthcare. Telehealth interventions such as the VA Video Connect app can greatly increase access to care for the more than 33,000 Veterans who are experiencing homelessness 4and is a modality Veterans experiencing homelessness with SUD prefer, 5 but research has found only moderate use of clinical video visits among homeless Veterans, with visit likelihood further reduced among those with SUD. 6
Between April 2015 and October 2022, more than 35,000 Veterans with a history of housing instability received VA-loaned tablets pre-loaded with the VA Video Connect telehealth app, a wireless service plan, and mobile connectivity. With few limits, Veterans could use the tablets to access resources at VA and beyond, such as housing services, food pantries, clothing, and job search sites.
This StudyBuilding on their prior research, investigators in this study (conducted from January to December 2021) sought to design an intervention tailored to Veterans experiencing homelessness with SUD to promote their use of video visits. The study was informed by the Unified Theory of Acceptance and Use of Technology model’s four use determinants of usefulness, ease/convenience, social influences, and facilitating conditions, and consisted of three phases:
* Listen to a recent HSR&D podcast in which Lynn Garvin discussed this study. Study Participants
FindingsPhase One ResultsVeteran interviews revealed that barriers to video telehealth included complex physical and mental health problems, a lack of digital literacy, and insufficient technical support. There were success stories, however. For example, one Veteran with a disability said that his tablet password had been pre-set so that he would not need to alternately type upper- and lowercase letters: “The [tablet] password was lowercase only because I have a hard time going back and forth on the iPad.” Ease of use and convenience were frequently cited advantages of video visits, but perceived complexity of the VA Video Connect app and tablets posed adoption barriers for some. Comments included: “VA needs to make the iPad as easy to use as the telephone.” “The links to the visits used to be confusing. Now, they’re better.” Lack of internet connectivity or privacy in Veterans’ living area were other barriers: “Where I live, the walls are thin; sounds travel.” Among those who were able to operate the tablets they received, Veterans appreciated their tablets’ reliability, generous data plan, and internet connectivity, which surpassed that of other devices the Veterans owned. One Veteran remarked: “I am comfortable with the iPad and like to have a [video] visit with my doctor because we can see each other. It is person-to-person. You’re not just on the phone.” Veterans who were living in VA-supported residences often reported living alone, without much interaction with family, friends, or the community. The video visits reduced isolation through connection with VA providers and offered “a feeling of being heard and understood,” said one Veteran. The greatest need for improvement voiced by Veterans experiencing homelessness with SUD was the perceived lack of VA support for training and adoption. Said one Veteran: “I can’t figure out how to work [the tablet] as far as setting it up.” Veterans called for improvements to address confusion with the visual layout of apps on the tablet’s opening screen, lack of awareness of VA Help Desk phone support, and lack of tablet training for Veterans and providers. One Veteran recalled: “I think [the tablet] arrived in the mail and I think I was told to call a number. This lady kind of explained a brief overview of some of the apps that were on there, and that was it.” The most frequent solution suggested by Veterans was digital skills training provided by VA-employed peer specialists. As one Veteran explained: “When you’re dealing with people that are somewhat ignorant to technology, . . . then they are lost. . . . I think we need more peer support. . . . You’re going to trust it if you’re hearing it from one of your peers.” Phase Two ResultsVeterans and provider experts proposed five intervention options to increase use of video telehealth among Veterans experiencing homelessness with SUD (Table 1). 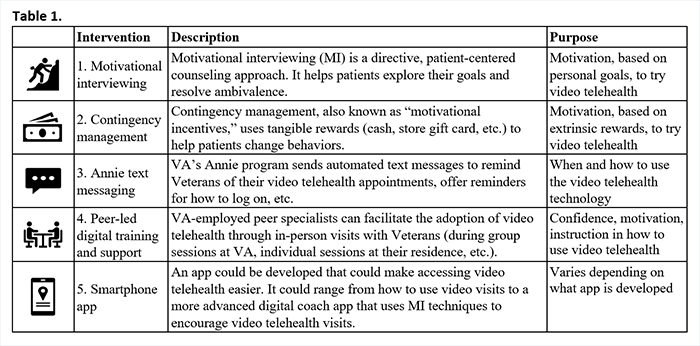
As Veteran focus group members discussed the options, their comments included the following: “I have a bad memory. Texts remind me about appointments.” “Texts are annoying.” “I found peer support very helpful during a period of bereavement. . . . I have a friend who is not computer savvy. He got some peer training on his tablet that helped him. But he needed multiple visits. You can’t expect some folks to pick it up on the first try.” Following the discussion, focus group members favored combining peer-led digital training and support with motivational interviewing. One Veteran observed: “Vets respond to someone like them. Vets feel it’s worth their time if a peer specialist will talk them through [the digital training]. . . . They need the coaching.” Phase Three ResultsResearchers designed a peer-led intervention prototype (Fig. 1) that can be adapted for group or individual use and trains and activates Veterans at all skill levels, providing increasing support for those who need it. 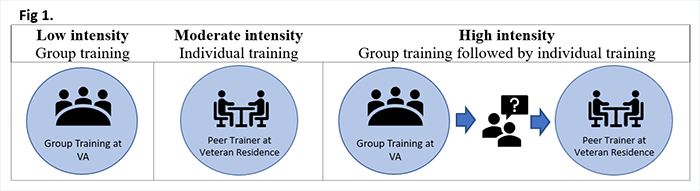
ImplicationsThis study demonstrates how expert and Veteran views contributed to the design of a tailored intervention to support and sustain use of video telehealth by Veterans experiencing homelessness with SUD. The intervention supports VA’s broader commitment to health access and health equity through expansion of digital literacy, and findings may have implications and benefits for other patient groups who face access barriers due to mental and behavioral health conditions, age-related ailments, or other conditions.
Study Publication Garvin L, Greenan M, Edelman E, et al. Increasing use of video telehealth among Veterans experiencing homelessness with substance use disorder: Design of a peer-led intervention. Journal of Technology in Behavioral Science. December 21, 2022;1–12. 1 History of co-occurring disorders and current mental health status among homeless veterans | BMC Public Health | Full Text (biomedcentral.com) 2 Disparities in Access to Medications for Opioid Use Disorder in the Veterans Health Administration - PubMed (nih.gov) 3 The Opioid Epidemic In Veterans Who Were Homeless Or Unstably Housed - PubMed (nih.gov) 4 Point-in-Time (PIT) Count - VA Homeless Programs 5 Patient Perceptions of Video Visits Using Veterans Affairs Telehealth Tablets: Survey Study - PubMed (nih.gov) 6 Use of Video Telehealth Tablets to Increase Access for Veterans Experiencing Homelessness - PubMed (nih.gov) |