
|
|
Research HighlightIdentifying Gaps in Veterans Health Administration (VHA) Distribution of Lifesaving NaloxoneVHA’s Naloxone EffortsIn 2022, drug overdoses claimed more than an estimated 100,000 lives in the United States, with opioids accounting for three quarters of these tragic deaths.1 To address this escalating crisis, in 2014, VHA launched the first national healthcare-based Opioid Overdose Education and Naloxone Distribution (OEND) program in the United States;2 this program not only disseminated naloxone, a life saving medication for reversing opioid overdoses, but also prioritized educating patients about opioid overdose prevention and response. In 2018, VHA expanded its naloxone efforts with a Rapid Naloxone Initiative to further prevent opioid overdose deaths among Veterans via a three-pronged approach: (1) providing OEND to VHA patients at risk for opioid overdose; (2) equipping VA Police with naloxone; and (3) equipping select automated external defibrillator cabinets with naloxone. This initiative received the 2020 John M. Eisenberg National Level Innovation in Patient Safety and Quality Award from The Joint Commission and the National Quality Forum,3 which recognizes major achievements to improve patient safety and healthcare quality. Given the large amount of VHA resources invested in naloxone and the need for rigorous evaluation of its effectiveness, HSR&D funded our team to examine the Effectiveness of a Rescue Medication in Preventing Opioid Overdose in Veterans (IIR 16-078; PI: Oliva). This article will focus on gaps in naloxone distribution, and specifically, opportunities for VHA to improve its efforts. Gaps in VHA Naloxone DistributionOur study characterized naloxone distribution to VHA patients diagnosed with an opioid use disorder (OUD) or prescribed an opioid analgesic (opioid Rx) between fiscal years 2014 through 2021 (FY2014-2021; 8 FY cohorts). We examined patient- and setting-level characteristics associated with naloxone receipt using generalized linear mixed models. This report focuses on the most recent FY2021 cohort. In FY2021, there were 627,687 VHA patients with an OUD or active opioid Rx (89 percent opioid Rx-only, 8 percent OUD-only, 3 percent OUD+opioid Rx) – mean age 63 years old – of whom 122,856 (20 percent) received naloxone. Naloxone receipt ranged from 15 percent among patients with an opioid Rx, 53 percent among patients with OUD-only, and 60 percent among patients with both OUD and an opioid Rx. Our cohort was predominantly male (90 percent), non-Hispanic (90 percent), and White (72 percent) with 64 percent living in urban settings, 35 percent in rural settings, and 1 percent in highly rural settings. Blacks comprised 19 percent while American Indians/Alaskan Natives, Native Hawaiian, Pacific Islanders, and Asians each comprised less than 1 percent of our cohort. Regarding opioid prescriptions, 70 percent received short-acting opioids (48 percent <90-day supply; 22 percent ≥90-day supply), 24 percent received tramadol only, and 6 percent received long-acting opioids. Major depressive disorder (28 percent), PTSD (26 percent), anxiety disorder (unspecified; 16 percent), nicotine use disorder (14 percent), and alcohol use disorder (11 percent) were the most common mental health and other substance use disorders. Past year healthcare utilization included 99 percent primary care, 47 percent outpatient mental healthcare, 45 percent emergency room (ER), and 27 percent surgery. We identified key gaps in naloxone distribution regarding sex, race, ethnicity, and healthcare utilization (see figure below). Females were less likely than males to receive naloxone (17 percent versus 20 percent). Regarding race and ethnicity, Asians and Blacks were less likely than Whites to receive naloxone (10 percent and 18 percent, respectively, versus 20 percent) and Hispanics were less likely than non-Hispanics to receive naloxone (16 percent versus 20 percent). Regarding healthcare utilization, VHA patients who utilized surgery, women’s health, and ER services were less likely to receive naloxone compared to those who did not (12 percent versus 22 percent; 16 percent versus 20 percent; and 18 percent versus 21 percent, respectively). Opportunities to Improve VHA Naloxone DistributionThis study identified opportunities to improve equitable VHA naloxone distribution by targeting specific patient populations and healthcare settings. Specific patient populations to target include females as well as Black, Asian, and Hispanic patients. Healthcare settings to target include surgical, women’s health, and ER services. The gaps identified for Black, Hispanic, and Asian patients are especially concerning given rising drug overdose mortality rates among these groups. Importantly, two years ago, we shared preliminary findings showing similar patterns through FY2019 with our advisory board (comprised of leaders across key VHA program offices including Pain Management, Office of Mental Health and Suicide Prevention, Pharmacy Benefits Management Services, and Emergency Medicine). VHA has already implemented initiatives to address identified gaps including an OEND Health Equity Dashboard which allows facilities to target OEND efforts based on age, sex, race/ethnicity, rurality, and special populations (e.g., potentially homeless, justice-involved) as well as an Emergency Department Opioid Safety Initiative that includes a dashboard to track naloxone distribution by at-risk Emergency Department/Urgent Care Center patients (includes patients in our cohort). Overall, only 1 in 5 patients with OUD or an opioid prescription received naloxone, suggesting broader efforts are needed. Risk-based prescribing occurred with more than half of patients with OUD as well as half of patients prescribed long-acting opioids receiving naloxone. Given the lack of data supporting broad co-prescribing of naloxone among patients prescribed opioids, it is possible that low rates of naloxone receipt among surgical patients reflect the perception that patients receiving short course opioids are low risk. Supporting risk assessment and targeted naloxone distribution to this large group – comprising almost half of our cohort (~300,000 patients) – may be important, especially given that the Comprehensive Addiction and Recovery Act of 2016 requires VHA providers, as part of a comprehensive assessment before initiating opioid therapy, to use a tool to assess risk for adverse outcomes of opioid therapy. Moreover, VHA’s memorandum Naloxone Distribution to Veterans at High-Risk also supports targeted naloxone distribution to patients with OUD, stimulant use disorder, a previous opioid or stimulant overdose, as well as very high risk VHA Stratification Tool for Opioid Risk Mitigation patients prescribed opioids. Overall, our study identified additional opportunities for VHA to further improve equitable access to naloxone. 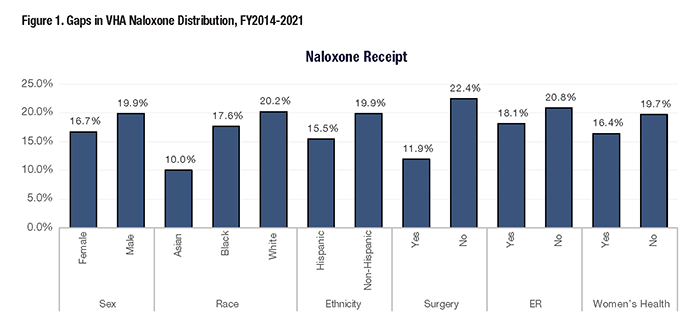
References
|
|