Telehealth is an effective and convenient way for patients to receive, and clinicians to provide, care. Telehealth leverages computer- and telephone-based technology in concert with health informatics, specialty care, and case management to improve care access, delivery, and quality. For example, telehealth can help improve the quality of care when primary care providers use real-time video to seek advice from specialists on diagnoses or procedures. Telehealth can also enhance Veterans’ and caregivers’ involvement in treatment through web-based applications such as MyHealtheVet that provide Veterans with access to their medical records and allow communication with the healthcare team.
VA was an early adopter of telehealth technology and remains committed to increasing access to care for Veterans, especially those in rural locations. In VA, telehealth programs have been developed, or are currently under development, for more than 50 specialty areas of care, including TeleAddiction, TeleAudiology, TeleCardiology, TeleDermatalogy, TeleMental Health, TeleMOVE! Weight Management, TelePrimary Care, and TeleStroke. VA Telehealth Services makes it easier for Veterans—whether they are at home or in a clinic or hospital—to connect with their VA care team and access high-quality care when and where they need it.
In addition, VA researchers at Health Services Research & Development (HSR&D) centers such as the Health Equity and Rural Outreach Innovation Center (HEROIC) and the Center for Health Information and Communication (CHIC) study innovations that enhance access to care, while a number of Quality Enhancement Research Initiative (QUERI) programs, such as the eHealth Partnered Evaluation Initiative, EXTEND, and Virtual Care QUERI, promote the advancement of telehealth in VA and the use of emerging virtual care technology to improve Veterans’ access to care. QUERI also works with several operations partners, including VA’s Office of Mental Health and Suicide Prevention and the VISN 1 Telemental Health Regional Hub, to develop and test materials and procedures that facilitate medication-assisted treatment delivery via telemedicine to Veterans at community-based outpatient clinics across the VA New England Healthcare System.

©iStock/yamasan
The suicide rate among Veterans is 50% higher than that in the general population and is disproportionately high among rural residents, a concerning pattern as the COVID-19 pandemic has intensified suicide risk factors in remote regions and exacerbated barriers to mental healthcare access. Although telehealth has the potential to improve access to mental healthcare, telehealth’s effect on suicide-related outcomes remains relatively unknown.
About this study
This study evaluated the association between the distribution of video-enabled tablets during the COVID-19 pandemic and rural Veterans’ mental health service use and suicide-related outcomes. Researchers compared monthly mental health service use among 13,180 patients who received VA tablets between March 16, 2020, and April 30, 2021, with 458,611 patients who were not issued tablets. The study included Veterans in rural settings who had at least one VA mental healthcare visit in 2019 and a sub-cohort of VA patients identified as high-risk for suicide.
Findings
Expected impacts
Principal investigator
 Kritee Gujral, PhD, is an investigator with HSR&D’s Center for Innovation to Implementation (Ci2i) and the Health Economics Resource Center (HERC).
Kritee Gujral, PhD, is an investigator with HSR&D’s Center for Innovation to Implementation (Ci2i) and the Health Economics Resource Center (HERC).
Publications
Gujral K, Van Campen J, Jacobs J, et al. Mental health service use, suicide behavior, and emergency department visits among rural US veterans who received video-enabled tablets during the COVID-19 pandemic. JAMA Network Open. April 6, 2022;5(4):e226250.
Oh A, Scott J, Gujral K, et al. Rural and urban differences in the implementation of virtual integrated patient-aligned care teams. The Journal of Rural Health. May 25, 2022; online ahead of print.
Gujral K, Scott J, Ambady L, et al. A primary care telehealth pilot program to improve access: associations with patients’ healthcare utilization and costs. Telemedicine and e-Health. May 11, 2022;28(5):643–653.
©iStock/Gam1983
Although efforts by clinicians and researchers have improved diabetes control across the VA healthcare system, many Veterans continue to struggle with persistently poorly controlled diabetes mellitus (PPDM) despite receiving clinic-based diabetes care. Veterans who experience PPDM—approximately 12% of all Veterans with type 2 diabetes—can have poor outcomes and contribute disproportionately to VA's burden of diabetes complications and costs. While clinic-based care is not sufficiently effective for PPDM, telehealth-based management that comprehensively addresses factors underlying PPDM could improve outcomes for these high-risk Veterans. But for telehealth to reduce PPDM, interventions must be developed with an emphasis on feasible implementation and delivery through the existing workforce, infrastructure, and technical resources.
About this study
This study evaluated a novel, comprehensive telehealth intervention for Veterans with PPDM designed for practical delivery within VA. Investigators aimed to:
In this study, 200 Veterans with PPDM were randomized to receive one of two Home Telehealth (HT)-delivered interventions: 1) a comprehensive intervention that combines telemonitoring; medication management; and support for self-management, diet, activity, and depression; or 2) standard HT care coordination and telemonitoring. Both interventions were delivered over a 12-month period and all participants continued to receive usual VA care. Intervention costs were comprehensively assessed and compared to standard HT care coordination and telemonitoring.
Findings
Expected impact
Because this study’s comprehensive telehealth intervention was designed for delivery via existing VA staffing and infrastructure, it may represent a practical approach that, for a reasonable additional cost, improves outcomes for Veterans with PPDM and reduces VA’s overall diabetes burden.
Principal investigator
 Matthew Crowley, MD, is part of HSR&D’s Center of Innovation to Accelerate Discovery and Practice Transformation (ADAPT) in Durham, NC.
Matthew Crowley, MD, is part of HSR&D’s Center of Innovation to Accelerate Discovery and Practice Transformation (ADAPT) in Durham, NC.
Publications
Crowley M, Tarkington P, Bosworth H, et al. Effect of a comprehensive telehealth intervention vs. telemonitoring and care coordination in patients with persistently poor type 2 diabetes control. JAMA Internal Medicine. September 1, 2022;182(9):943–952.
Kobe E, Edelman D, Crowley M, et al. Practical telehealth to improve control and engagement for patients with clinic-refractory diabetes mellitus (PRACTICE-DM): Protocol and baseline data for a randomized trial. Contemporary Clinical Trials. November 2020;98:106157.

©iStock/gerenme
Amid a national opioid epidemic, opioid use disorder (OUD) prevalence in Veterans has increased. Many Veterans with OUD experience serious and preventable harms including overdose and suicide. The medication buprenorphine can help prevent these harms, but only a third of Veterans with OUD receive this evidence-based treatment. Treatment barriers include a lack of trained buprenorphine providers, stigma of OUD, and limited accessibility of care. Telehealth interventions have been developed in VA that have expanded treatment for numerous chronic conditions, but minimal research has been done on telehealth for substance use disorders.
About this study
This ongoing (April 2019–March 2024) HSR&D study, while adapting to the impacts of COVID-19 and the dramatic expansion of telehealth use, addresses a critical VA and HSR&D priority to improve access to OUD treatment by developing and testing a telehealth treatment delivery intervention. Investigators aim to:
Findings
None yet available.
Expected impacts
Principal investigator
 Lewei (Allison) Lin, MD, MS, is an HSR&D Career Development Awardee and part of HSR&D’s Center for Clinical Management Research (CCMR) in Ann Arbor, MI.
Lewei (Allison) Lin, MD, MS, is an HSR&D Career Development Awardee and part of HSR&D’s Center for Clinical Management Research (CCMR) in Ann Arbor, MI.
Publications
Frost M, Zhang L, Kim H, Lin L. Use of and retention on video, telephone, and in-person buprenorphine treatment for opioid use disorder during the COVID-19 pandemic. JAMA Network Open. October 12, 2022;5(10):e2236298.
Frank C, Lin L. Defining and supporting high-quality telehealth for patients with opioid use disorder: the promise and potential pitfalls of telehealth expansion. Substance Abuse Journal. October 12, 2022;43(1):1370–1373.
Lin L, Zhang L, Kim H, et al. Impact of COVID-19 telehealth policy changes on buprenorphine treatment for opioid use disorder. The American Journal of Psychiatry. July 28, 2022;online ahead of print.
Lin L, Fortney J, Bohnert A, et al. Comparing telemedicine to in-person buprenorphine treatment in US veterans with opioid use disorder. Journal of Substance Abuse Treatment. February 1, 2022;133:108492.

©iStock/PeopleImages
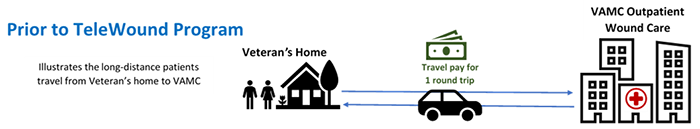
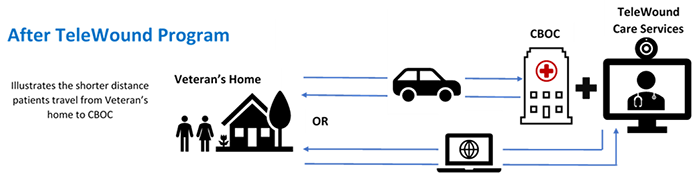
Chronic wounds such as pressure injuries and diabetic foot ulcers are a significant predictor of mortality among Veterans. The TeleWound Practice (TWP) program, a coordinated effort within VA to provide wound care to Veterans using telehealth technologies that enhance access to specialty wound care—especially for Veterans who live in rural areas—was selected for regional rollout as part of the VA Shark Tank Competition. An early pilot of TWP suggests that delivering TeleWound care may reduce Veteran travel time and costs related to wound care, and that Veterans who received TeleWound care were satisfied with it.
About this study
QUERI’s TeleWound Practice Partnered Evaluation Initiative aims to assess the implementation and effects of TWP on clinical and healthcare system outcomes. It joins national, regional, and local health system leaders to evaluate the four VA facilities from VISN 15 (also known as the VA Heartland Network) and their community-based outpatient clinics (CBOCs) that are participating in the initial implementation of TWP.
QUERI investigators are conducting their evaluation of TWP through:
Findings
Once a week I’ll take a picture of my wound and send it in. They can look at it and say, ‘Oh, yeah, it looks like it’s doing this’ or ‘Do we want to do that.’ It’s more interactive in the wound care itself. It gets the patient more involved with wound care than [leaving] everything to the doctor.”—TWP patient
Expected impact
Evaluation of the TWP rollout in VISN 15 identified barriers and solutions to TeleWound implementation in a small number of sites, which can be used to inform successful rollout of the TWP nationally and result in improved Veteran access to wound care and reduced travel burden and costs for Veterans.

Frances M. Weaver, PhD, MA (left) Bella Etingen, PhD, MA (right) |
Principal investigators: Frances M. Weaver, PhD, MA, is an HSR&D Research Career Scientist and part of HSR&D’s Center of Innovation for Complex Chronic Healthcare (CINCCH) at the Hines VA Hospital in Hines, IL, along with Bella Etingen, PhD, MA. |
Publications
Kostovich C, Etingen B, Wirth M, Weaver F, et al. Outcomes of telehealth for wound care: A scoping review. Advances in Skin & Wound Care. July 1, 2022;35(7):394–403.
Etingen B, Amante D, Martinez R, et al. Supporting the implementation of connected care technologies in the VHA: cross-sectional survey findings from the Veterans Engagement with Technology Collaborative (VET-C) cohort. Journal of Participatory Medicine. September 30, 2020;12(3):e21214.
Etingen B, Patrianakos J, Weaver F, et al. TeleWound practice within the Veterans Health Administration: Protocol for a mixed methods program evaluation. JMIR Research Protocols. July 20, 2020;9(7):e20139.