
|
|
CommentaryUsing Data, Tools, and Technology to Improve the Patient ExperienceThe implementation of the VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018 (MISSION Act), empowered Veterans with more health care options and strengthened the nationwide VA healthcare system. VA Secretary Robert Wilkie, OMR, recently stated that the MISSION Act “put[s] Veterans at the center of their care and offer[s] options, including expanded telehealth and urgent care, so they can find the balance in the system that is right for them.” In line with the MISSION Act priorities, the Veterans Experience Office (VEO) puts the Veteran at the center of everything we do, through Veteran- centered designs and the implementation of industry best practices. VEO leverages data, tools, and technology to enable VA to be the leading customer service organization in government. VEO and the Veterans Healthcare Administration (VHA) further define the patient experience (PX) as, “the sum of all interactions, shaped by the organization’s culture, that influence Veterans’ and their families’ perceptions along their healthcare journey.” Patient experience is the organizational alignment of people, processes, and culture around the common goal of creating a consistent, exceptional experience for Veterans, their families, caregivers, and survivors. In 2017, the call for a dedicated review of the patient experience identified inconsistent approaches and experiences across VA. An article in JAMA Internal Medicine stated, “VA hospitals performed better than non-VA hospitals…[but] performed worse on certain patient experience measures and behavioral health measures” (JAMA Internal Medicine, April 2017). The review led to efforts to standardize and improve the patient experience through a partnership with VHA and VEO’s Veterans Patient Experience (VA PX) team. Since 2017, VA serves as the Lead Agency Partner for the President’s Management Agenda (PMA) Cross-Agency Priority (CAP) Goal on improving the customer experience federal government-wide. VA included the importance of the customer experience in the Code of Federal Regulations (38 CFR § 0.603): “VA will provide the best customer experience in its delivery of care, benefits, and memorial services to Veterans, service members, their families, caregivers, and survivors. The delivery of exceptional customer experience is the responsibility of all VA employees and will be guided by VA’s Core Values and Characteristics. Customer experience is the product of interactions between an organization and a customer over the duration of their relationships. VA measures these interactions through Ease, Effectiveness, and Emotion, all of which impact the overall trust the customer has in the organization.” The VA Patient Experience framework guides products, research, and technological development of tools to improve the patient experience across VHA. The framework can help identify opportunities for improving individual measures of Veterans’ overall patient experience and the cultural feeling of trust. 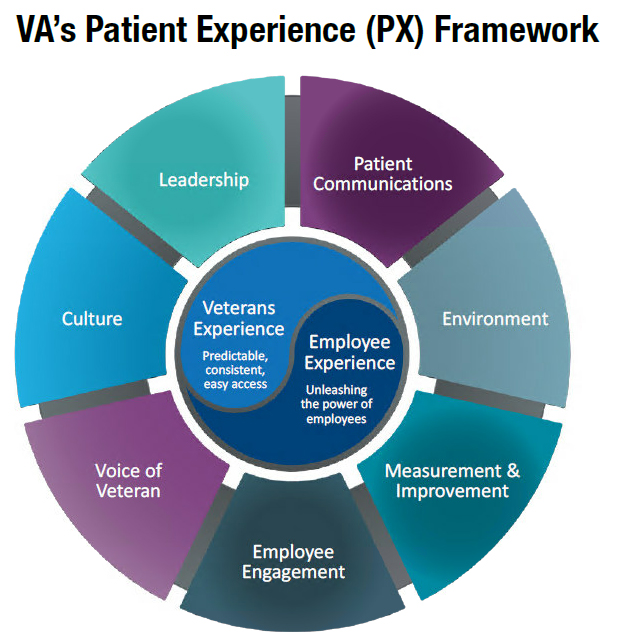
Journey MapsCentral to the solutions and tools being implemented to improve the patient experience across VA is the utilization of human-centered design (HCD). HCD is an innovative approach to problem solving and solutions development. The HCD approach ensures the Voice of the Veteran and Voice of the Employee are captured and allows VA to identify the moments that matter most to Veterans, their families, caregivers, and survivors. Journey maps represent a common set of moments that matter most to Veterans throughout the various phases of their interaction with VA. Journey maps identify both bright spots (things VA does well) and pain points (areas where VA needs to improve). By using journey maps, VA is able to visualize the end-to-end journey and have the opportunity to identify and align high impact patient experience improvement efforts across the entire VA system. Since 2017, VEO has published a number of VHA journey maps including, but not limited, to the: inpatient discharge journey, inpatient hospitalization journey, outpatient journey, and outpatient women Veterans journey. Additional journey maps are in development. Foundational ToolsFrom 2017 to 2019, VA PX implemented five foundational tools across VHA healthcare systems to assist with the standardization of branded and positive orchestrated touchpoints that lead to improved patient experiences and trust in VA. VA PX designed the foundational tools to improve interactions identified as the outpatient moments that matter most to patients in their outpatient journey. The foundational tools align to lead change across our VA culture, people, and processes. By engaging leaders and employees, creating a culture of caring and clear communication, and measuring and improving our qualitative and quantitative research, we can improve VA’s patient experience. VA employees are required to learn how to facilitate positive customer experiences through the Own the Moment (OTM) workshop. In OTM, employees learn guiding principles aligning ease (making it easy), effectiveness (understanding and responding to needs), and emotion (feeling like a valued customer). 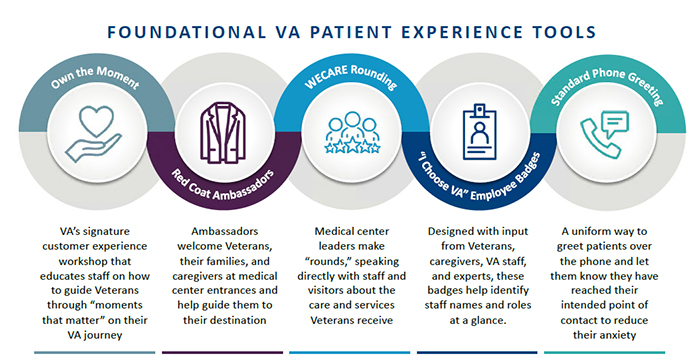
Measuring the Patient ExperienceTo understand the overall experience and trust in VA, we utilize the Veterans Signals (VSignals) and Survey of Healthcare Experiences of Patients (SHEP) survey mechanisms. This quantitative data provides a balance to the utilization of the more human-centered design focus of qualitative data. VA has an opportunity to gain trust by adding emotion into our interactions, building stronger relationships, recommitting to our shared purpose of caring for Veterans, and showing that they are our valued customers. As VA adapts and innovates to facilitate healthcare for Veterans in a pandemic and post-pandemic era, we need to learn:
References
|
|
Next ❯