Takeaway: These HSR&D studies evaluated quality and patterns of lung cancer screening (LCS) nationally in VA. Findings are informing implementation of a personalized approach to optimize equity and patient-centeredness of lung cancer screening (LCS) and facilitate shared decision-making between Veterans and VA clinicians. Two measures from this work were adopted by VA’s National Center for Lung Cancer Screening as LCS quality metrics. Also, in response to this work and other considerations, VA is now drafting a Directive to require all VA facilities to offer LCS.
The American Cancer Society estimates that approximately 127,070 U.S. adults (67,160 men and 59,910 women) will die from lung cancer in 2023. Moreover, there will be about 238,340 new cases (117,550 men and 120,790 women) of lung cancer among U.S. adults.1 Nearly 8,000 Veterans are diagnosed and treated for lung cancer in the VA healthcare system every year. Veterans have higher risk for lung cancer due to older age, smoking, and environmental exposure during and after military service. Overall, Veterans have a higher rate of lung cancer and a lower rate of survival than the general population.2 However, two large randomized controlled trials demonstrated that diagnosing early-stage lung cancer with low-dose computed tomography (CT) screening reduces death from lung cancer by approximately 20% among high-risk individuals. 3,4
Lung Cancer Screening
The U.S. Preventive Services Task Force (USPSTF) recommends annual screening for lung cancer with low-dose CT in adults aged 50 to 80 years who have a 20 pack-per-year smoking history and currently smoke or have quit within the past 15 years. Screening should stop once a person has not smoked for 15 years, or develops a health problem that substantially limits life expectancy or the ability/willingness to have curative lung surgery.5 VA follows the USPSTF guidelines for LCS, and it is estimated that more than one million Veterans are eligible for LCS by these criteria.
Implementing lung cancer screening (LCS) is a VA priority, but little was known about LCS quality in VA practice. Renda Wiener, MD, MPH – a pulmonary and critical care physician and Associate Director of HSR&D’s Center for Healthcare Organization & Implementation Research (CHOIR) in Boston, MA – led an HSR&D study (IIR 18-075) to:
Findings
Results of this study showed uneven access to lung cancer screening and uptake across VA (see Figure below). In addition, while Black and Hispanic Veterans were more likely to accept LCS when it was offered, Black Veterans with mental health or substance use disorders, those with lower income, and those who live further from VA were more likely to have delayed or absent follow-up after initiating LCS. These findings suggest that additional resources are needed to support the uptake and adherence to LCS to prevent widening of lung cancer disparities.
![Figure: Uneven access to and uptake of LCS across VAMCs, 2013-19. Source: Boudreau et al, <em>Chest, </em>2021. [Darker shading indicates greater screening in VA per 10,000 eligible.]](uneven-access-LCS.png)
Figure: Uneven access to and uptake of LCS across VAMCs, 2013-19. Source: Boudreau et al, Chest, 2021. [Darker shading indicates greater screening in VA per 10,000 eligible.]
Shared-Decision Making for Lung Cancer Screening
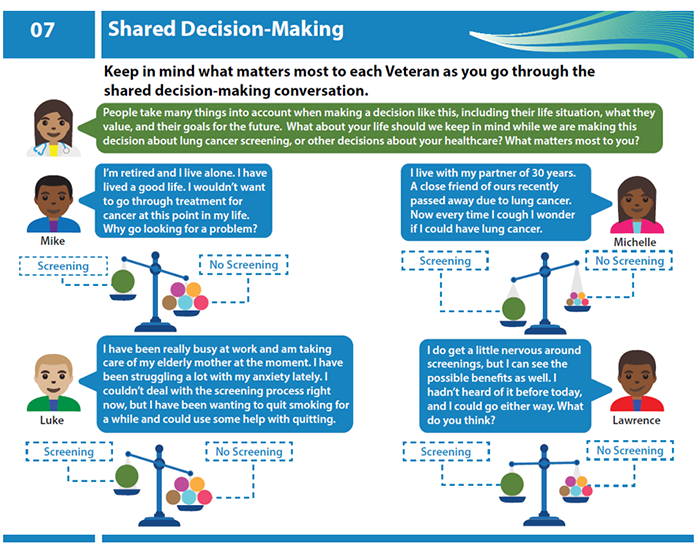
Dr. Wiener and Gemmae Fix, PhD – a CHOIR investigator and former HSR&D Career Development Awardee – also led an HSR&D RIVR (Research to Impact for VeteRans) project to implement shared decision-making (SDM) for LCS across VISN 1 (VA New England Healthcare system). SDM—a process to determine if LCS is the right choice for an individual patient based on their values, goals and preferences—is required by Medicare and recommended by VA. This prospective study identified barriers to SDM for LCS at each level of the socioecological model, including system, provider and patient levels. Findings were then used to develop a tailored, multilevel approach to implementing SDM for LCS across VISN 1 (VA New England Healthcare System) by leveraging the existing patient-centered, Whole Health culture.
At the provider level, the team used academic detailing and interactive training of VISN 1 LCS coordinators in tailoring SDM conversations so that they would take into account Veterans’ values and goals (see Figure for sample from academic detailing materials).
At the patient-level, the team co-designed, with Veterans, a patient-facing booklet to empower Veterans to participate in SDM for LCS. Finally, the team will evaluate implementation of this multilevel approach and its impact on effectiveness (primary outcome, defined as patient-centeredness of SDM). Tailored implementation will:
Future directions
Drs. Wiener and Fix, along with Ms. Anna Barker (CHOIR), are expanding this work to meet Veterans where they are. In her newly funded HSR&D pilot project (PPO 22-161), Dr. Wiener will co-design and pilot-test a Veteran peer-led intervention of community outreach, education, and navigation to engage Black Veterans in lung cancer screening. In addition, as part of an ORD-funded project conducted in conjunction with HSR&D investigators Nichole Tanner, MD, (HSR&D’s Health Equity and Rural Outreach Innovation Center) and Tanner Caverly, MD, (HSR&D’s Center for Clinical Management), Dr. Wiener is leading a study to develop and pilot test a proactive outreach approach to engage Veterans with high predicted benefit from LCS in screening, to improve equity of LCS and optimize resource use. This project is being conducted in collaboration with the VA Lung Precision Oncology Program (LPOP).
Implications
To maximize the life-saving potential of lung cancer screening without creating additional harms and wasting VA resources, LCS must be applied equitably and with attention to individual Veteran’s values, preferences, and predicted net benefit from LCS. These studies can inform future development, testing, and implementation of a personalized approach to optimize patient selection for LCS and facilitate shared decision-making between Veterans and VA clinicians at the point-of-care.
As a result of this body of work, Dr. Wiener was appointed Deputy Chief Consultant of the National Center for Lung Cancer Screening – tasked with drafting VA LCS Directive to require all VA facilities to offer LCS. Also, two measures from this work were adopted by VA’s National Center for Lung Cancer Screening (NCLCS) as LCS quality measures.
References
Publications
Boudreau J, Miller D, Qian S, et al. Access to lung cancer screening in the Veterans Health Administration: Does geographic distribution match need in the population? Chest. July 2021;160(1):358-367.
Khanna A, Fix G, McCullough M, et al. Implementing shared decision-making for lung cancer screening across a Veterans Health Administration hospital network: A hybrid effectiveness-implementation study protocol. Annals of the American Thoracic Society. March 2022;19(3):476-483.
Núñez E, Caverly T, Zhang S, et al. Adherence to follow-up testing recommendations in US Veterans screened for lung cancer, 2015-2019. JAMA Network Open. July 2021;1;4(7):e2116233.
Wiener R, Barker A, Carter-Harris L, et al. Stakeholder research priorities to promote implementation of shared decision-making for lung cancer screening: An American Thoracic Society and Veterans Affaris Health Services Research and Development Statement. American Journal of Respiratory and Critical Care Medicine. March 2022;205(6):619-630.